The ultimate guide for Therapist-Made rehabilitation plans
Written by: Brianna Hodge
Imagine a world where therapy isn’t confined to four walls or limited by the availability of certain tools. Imagine being able to walk your patient through a busy crosswalk for gait training, or guide a stroke survivor through a virtual kitchen as they relearn daily tasks—all from the safety and control of your clinic. What if that world already existed?
Welcome to the future of rehabilitation: therapist-designed virtual reality (VR) experiences. And it’s not just about technology—it’s about you, the clinician, finally having the creative and clinical freedom to craft scenarios tailored to your patients’ exact needs.
From Passive User to Active Creator
Traditionally, therapy tools are built for therapists, but not by them. You get what’s available: balance boards, obstacle courses, flashcards, maybe a touchscreen game. VR changes that. Now, therapists aren’t just users—they’re creators.
Custom VR experiences allow you to tailor every aspect of an environment. You can adjust sensory input for patients with vestibular disorders, simulate real-world distractions for individuals with attention deficits, or design progressive environments for patients with PTSD to practice exposure therapy—all within a controlled, data-rich setting.
Research:
A recent systematic review titled Effect of Home-Based Virtual Reality Training on Upper Extremity Recovery in Patients With Stroke reinforces what many therapists already know: tailored care works best.
The review found that home-based VR training led to meaningful improvements in upper extremity motor control for stroke survivors—especially for those with moderate to severe impairments. But here's what really stood out: customized VR systems, the kind designed specifically for therapeutic use, outperformed commercial, off-the-shelf VR games. That distinction matters. It validates the role of therapists as designers—those who understand that rehab isn’t just about movement, but about creating the right environment, at the right time, for the right patient.
With the right tools, recovery doesn’t stop at the clinic door. It follows patients home, in ways that feel personal and purposeful.(Huang et al.)
Why Custom Scenarios Matter in Clinical Practice
Every patient is different. You know this more than anyone. A therapy that works wonders for one may overwhelm or under-stimulate another. So, why should we expect one-size-fits-all solutions?
Take gait training, for example. One patient may struggle with foot placement and balance, while another finds it difficult to navigate busy environments due to spatial disorientation or cognitive overload. Traditional methods, like walking a straight hallway or using a treadmill, rarely address these individual challenges in a meaningful way. But with VR, you can meet each patient where they are.
Research:
Every patient is different—and so is every therapist. That’s why usability isn’t just a feature in VR rehabilitation; it’s a foundational necessity. In the study The Dual Importance of Virtual Reality Usability in Rehabilitation: A Focus on Therapists and Patients, researchers emphasized how both patient and clinician experiences with VR shape its success.
For patients, especially those with neurological or motor impairments, intuitive interfaces and meaningful feedback loops can mean the difference between frustration and progress. For therapists, ease of scenario creation, session management, and data interpretation directly impacts workflow and long-term adoption.
When VR systems are thoughtfully designed with both groups in mind, prioritizing accessibility, clarity, and responsiveness - they become more than tools. They become extensions of the clinician’s expertise and amplifiers of the patient’s effort. Customizability, yes, but also usability, because good design meets people where they are, not where the technology wants them to be.(Naqvi et al.)
The Clinician's Creative Toolbox: What Can You Control?
With the right VR platform, here’s what you as a clinician can now manipulate:
Environment Type: indoors, outdoors, high stimulation, low stimulation.
Sensory Input: adjust noise, lighting, motion visuals.
Task Difficulty: from passive observation to dual-task performance.
Functional Objectives: reach, grasp, balance, navigate, plan.
Time & Progression: control the pace, stage tasks, or set up circuit training.
This level of control gives you the flexibility to simulate real-world tasks and document improvements in a way that static therapy cannot.
Evidence Speaks: What the Research Says
Research Study One:
Dual-task gait training is notoriously challenging for patients with Parkinson’s disease, yet it’s essential for maintaining independence and reducing fall risk. According to the systematic review Is virtual reality beneficial for dual-task gait training in patients with Parkinson's disease?, VR emerges as a powerful tool—not just for physical rehabilitation, but for boosting motivation and adherence.
The review highlights how VR-based training allows therapists to introduce cognitive challenges progressively, layering tasks in a way that’s both clinically strategic and engaging. Unlike traditional rehab, VR can turn repetition into exploration, offering personalized exercises that feel less like routine and more like accomplishment.
That blend of personalization and play is key, because when therapy is enjoyable and adaptive, patients are more likely to stick with it and push themselves further. (Freitag et al.)
Research Study Two:
As VR technology continues to evolve, its promise in cognitive rehabilitation is becoming harder to ignore. The narrative review Virtual Reality for the Rehabilitation of Acquired Cognitive Disorders outlines how VR offers a uniquely immersive and engaging avenue for addressing cognitive deficits following brain injury, stroke, or other neurological events.
What sets VR apart is its ability to deliver personalized interventions that simulate real-life challenges—such as planning a route through a city or remembering a grocery list—within a safe, controlled environment. This blend of realism and adaptability not only boosts engagement but also enables more accurate assessment and training of executive functions, attention, and memory.
While the review acknowledges that challenges remain, such as standardizing protocols and ensuring accessibility, the future is clearly pointing toward VR as a powerful, clinician-driven tool for reshaping how we approach cognitive recovery.
Together, these reviews highlight how personalized VR can transform rehab. Making it engaging, adaptable, and effective for both cognitive and motor challenges. When therapists design tailored experiences, therapy becomes more than routine—it becomes meaningful.
Case Study: Designing for Success – Trunk Control and Motion Amplification in VR
This patient story highlights exactly why therapist-designed VR experiences matter. A patient with an incomplete spinal cord injury struggled with poor trunk control and limited lateral spinal flexion. In traditional therapy, lateral weight shifts were minimal and discouraging—progress felt invisible, and the effort often led to a loss of balance. It was clear this patient needed more than standard repetition—they needed feedback that felt meaningful.
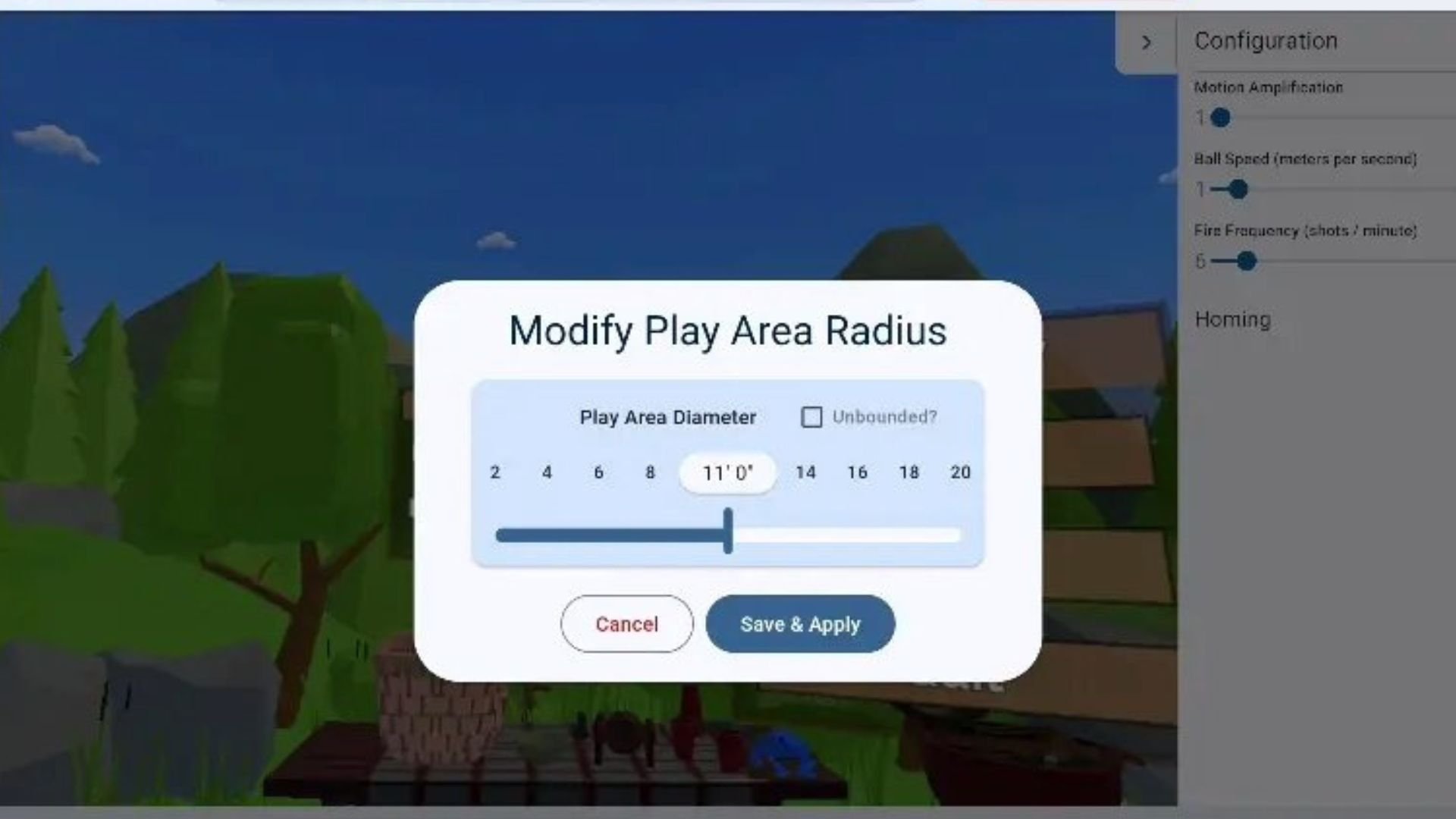
To meet that need, the therapist used a custom VR scenario featuring lateral reaching tasks. But instead of keeping the visuals one-to-one with real motion, they activated a motion amplification feature—one designed to make small trunk movements appear larger in the virtual environment. This personalized setting allowed the patient to see successful, dramatic side-to-side movement, even when their physical range was still limited.
The result? Engagement skyrocketed. The patient, now seeing success with every reach, became motivated to push further. More trunk movement followed. Balance improved. Confidence returned. And as the patient’s control grew, the therapist gradually dialed down the motion amplification, transitioning the experience to mirror real-world effort.
This scenario exemplifies how giving therapists the ability to adjust visual feedback and progression in VR can directly impact patient outcomes. It’s not about flashy tech—it’s about using tools that let clinicians customize, adapt, and build therapy that meets patients exactly where they are.
Neuro Rehab VR: Putting Power into the Hands of Clinicians
At Neuro Rehab VR, we’ve always believed therapists are the architects of recovery. That’s why our Smart Therapy Complete Solution doesn’t just offer pre-built games—it empowers you to design your own.
Using our clinician tablet interface, you can:
Select 360 environments (from a serene beach to the Eiffel tower).
Customize task types (e.g., fine motor vs. balance).
Adjust complexity in real time based on patient performance.
Integrate dual-task activities for cognitive-motor training.
Track data, modify plans, and export progress reports instantly.
What’s more, our solution is FDA-registered, HIPAA-compliant, and supports CEU-accredited training for clinicians to learn how to create these experiences responsibly and creatively.
Clinicians using our platform have reported not just patient progress, but renewed therapist motivation—because they’re no longer confined to the limits of traditional care.
Reducing Burnout Through Creative Engagement
Let’s talk honestly—clinician burnout isn’t just real, it’s widespread. According to a national survey published in 2023 and conducted by a team of APTA members, nearly 50% of physical therapists reported feeling burned out, with particularly high rates among those working in skilled nursing, home health, and outpatient settings.
The study, which gathered responses from over 2,800 PTs across nine states, found that burnout wasn’t distributed evenly. It was significantly lower among therapists who had access to mentorship and those who reported higher levels of self-efficacy—that sense of control and purpose in one’s work. It’s a powerful reminder: when therapists feel boxed in by rigid workflows, repetitive tasks, and limited autonomy, their passion fades. But when they’re given the tools to create—to personalize care, adapt treatments, and engage with patients in meaningful, dynamic ways—burnout doesn’t just decrease, engagement increases. (APTA)
Custom VR design puts that creativity and control back into the hands of the clinician. Instead of following a static program, therapists become architects of therapy—designing scenarios that reflect their clinical judgment and their patients’ real needs. That shift doesn’t just support patient outcomes. It supports the well-being of the people driving those outcomes every day.
Training Therapists to Think Like Designers
Of course, designing VR experiences requires training. That’s why smart rehab platforms include therapist education. But the learning curve is less about tech and more about mindset. You already know how to problem-solve for patients—it’s about translating that into 3D environments.
Courses on VR scenario design often teach:
Clinical storytelling: mapping real goals into VR narratives.
Accessibility considerations: for patients with visual, cognitive, or motor impairments.
Data-informed design: how to iterate based on patient response.
Ethics: balancing realism with patient safety and emotional well-being.
As you grow in your comfort with these tools, your ideas will expand too. You might build simulations for job reintegration, driving skills, or even social interactions in public places.
Barriers and Bridges: What Still Needs Work
This isn’t to say the road is without obstacles. Some common challenges include:
Reimbursement confusion: While CPT codes exist for therapeutic activity and cognitive training, not all payers accept VR-based equivalents yet.
Hardware limitations: Not all clinics have space or Wi-Fi that supports wireless VR.
Learning curve: Therapists need time and support to develop design skills.
Patient variability: Some patients experience motion sickness or visual confusion.
But with the rise of research-backed platforms, portable headsets, and clinician education, these barriers are shrinking. The key is collaboration between tech developers and clinicians—exactly what companies like Neuro Rehab VR are built on.
A Future Where Therapy Looks Like the Real World
As healthcare moves toward personalized medicine, rehabilitation must follow. The days of generic protocols are fading. In their place, we’re seeing a vision of therapy that is as dynamic as the human brain itself—customizable, experiential, and responsive.
You, as a clinician, are no longer just a guide. You are a builder of experiences. VR gives you the toolkit. Your clinical wisdom brings it to life.
And in that fusion, recovery doesn’t just happen, it’s accelerated.
Closing Thoughts: You Already Have What It Takes
If you’ve ever adapted a treatment plan on the fly, built rapport with a resistant patient, or found creative ways to meet goals in under-resourced settings—you’re already doing the hard part.
VR design is just a new medium for your clinical creativity. With platforms like Neuro Rehab VR supporting you, the question isn’t can you design these experiences. It’s what will you create first?
Because when therapy is crafted by those who understand the patient best—the clinician—everything changes.
-
APTA. “Research Review | Study: Nearly 50% of PTs Surveyed Say They’re Experiencing Burnout.” APTA, 15 Nov. 2023, www.apta.org/article/2023/11/15/burnout-survey.
Freitag, Fernanda, et al. “Is Virtual Reality Beneficial for Dual-Task Gait Training in Patients with Parkinson’s Disease? A Systematic Review.” Dementia & Neuropsychologia, vol. 13, no. 3, Sept. 2019, pp. 259–267, https://doi.org/10.1590/1980-57642018dn13-030002.
Huang, Jiaqi, et al. “Effect of Home-Based Virtual Reality Training on Upper Extremity Recovery in Patients with Stroke: Systematic Review.” Journal of Medical Internet Research, vol. 27, 4 Apr. 2025, p. e69003, pmc.ncbi.nlm.nih.gov/articles/PMC12008694/, https://doi.org/10.2196/69003. Accessed 2 May 2025.
Naqvi, Waqar M, et al. “The Dual Importance of Virtual Reality Usability in Rehabilitation: A Focus on Therapists and Patients.” Curēus, 22 Mar. 2024, www.ncbi.nlm.nih.gov/pmc/articles/PMC11032731/, https://doi.org/10.7759/cureus.56724.