Revolutionizing Rehab: A New Era of Patient Progress Tracking
Written by: Brianna Hodge
Rehabilitation is not just about the exercises—it’s about progress. For anyone undergoing physical or cognitive therapy, knowing that you’re getting better can make all the difference in staying motivated. But how do you truly measure improvement? Traditionally, progress tracking in rehabilitation has relied on subjective observations and intermittent assessments. While these methods have their place, they don’t always provide the full picture.
This is where virtual reality (VR) rehabilitation is changing the game. VR offers objective, data-driven tracking of patient outcomes, enabling both patients and therapists to see real-time progress. By incorporating motion capture, AI analytics, and immersive therapy, VR allows clinicians to assess fine motor improvements, cognitive responses, and adherence to treatment plans with unparalleled precision.
But what does the research say? Let’s explore how VR is transforming rehabilitation tracking and why it’s beneficial for both patients and therapists.
The Shift from Subjective to Data-Driven Assessment
For years, therapists have relied on functional tests, patient-reported outcomes, and clinical judgment to assess rehabilitation progress. These methods, while valuable, can be limited by observer bias, patient perception, and the inability to track subtle, day-to-day improvements.
A meta-review published in Bioelectronic Medicine (2024) examined multiple systematic reviews on virtual reality (VR) in stroke recovery, emphasizing VR’s role in accurately tracking patient progress. The study found that VR-based rehabilitation systems offer real-time data on motor function improvements, balance, and neuroplasticity, providing clinicians with quantifiable insights that traditional assessments often miss. By capturing detailed movement patterns and therapy adherence, VR enhances objective patient monitoring, allowing for more personalized and adaptive treatment plans. (Khan et al.)
By using VR-based rehabilitation tools, therapists can collect detailed movement metrics, including:
Reaction time to stimuli.
Speed and accuracy of movements.
Range of motion (ROM) and consistency.
Cognitive engagement levels during tasks.
This shift from guesswork to data-backed insights enables therapists to tailor rehabilitation plans more effectively, leading to better patient outcomes.
AI-Driven Documentation: Reducing Administrative Burden
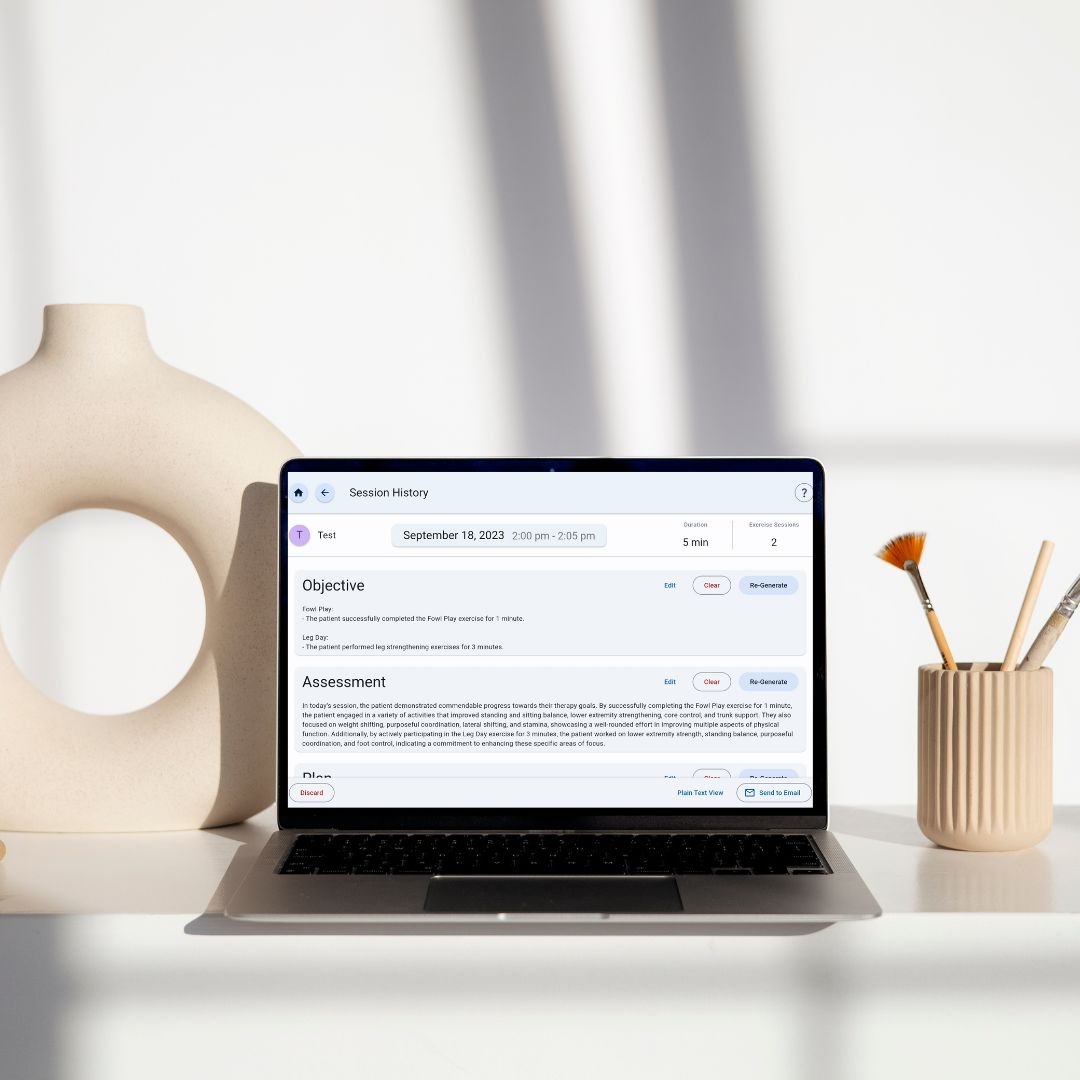
One of the biggest challenges in rehabilitation is documentation overload. A therapist’s day is often consumed with writing SOAP notes (Subjective, Objective, Assessment, and Plan), leaving less time for direct patient care. But AI-assisted automation, such as the Smart Therapy Complete Solution, is stepping in to solve this problem.
Smart Therapy Complete Solution takes AI-driven documentation to the next level by automating SOAP note generation with unparalleled accuracy. The system seamlessly integrates into therapy sessions, tracking patient progress in real-time and automatically compiling structured SOAP notes without requiring extensive manual input from therapists.
How it Helps:
Automated Movement Analysis: AI tracks therapy sessions and generates quantifiable reports based on patient progress.
Pre-Filled SOAP Notes: AI extracts key metrics and organizes them into standardized clinical documentation.
Real-Time Data Insights: Clinicians can access instant reports, helping them make faster, evidence-based decisions.
Research Insight:
A systematic review published in Artificial Intelligence in Medicine (2024) explored the integration of artificial intelligence (AI) in physical rehabilitation, emphasizing its role in enhancing patient tracking and treatment personalization. The study found that AI-driven rehabilitation systems improve real-time monitoring of patient progress, automate movement analysis, and provide predictive insights that help clinicians adjust therapy plans more effectively. By leveraging machine learning algorithms, AI enhances objective outcome tracking, reducing reliance on subjective assessments and improving rehabilitation efficiency (Sumner et al.)
Not only does Smart Therapy Complete Solution save therapists valuable time, but it also improves documentation accuracy, ensuring compliance with healthcare regulations and enhancing collaboration between providers.
Benefits for Therapists: Efficiency, Accuracy, and Compliance
1. Real-Time Progress Tracking
One of the most powerful features of VR-based rehabilitation is its ability to track continuous micro-improvements. Instead of waiting for scheduled assessments, therapists can see patient progress in real-time and adjust therapy accordingly.
For instance, patients recovering from traumatic brain injuries (TBIs) often struggle with coordination. VR systems can measure the speed and accuracy of limb movements, providing therapists with precise data to track improvements and adjust exercises.
2. Reducing Burnout and Enhancing Efficiency
Therapists often feel overwhelmed by excessive administrative tasks. AI-assisted tracking systems help by:
Reducing time spent on documentation.
Providing automated progress reports.
Minimizing repetitive paperwork.
With AI handling data analysis, therapists can focus on what matters most—direct patient care.
3. Improved Compliance and Reimbursement
Insurance reimbursement often depends on accurate documentation. With AI-generated clinical notes and VR-based outcome tracking, therapists can provide:
Objective proof of patient progress for insurance claims.
Data-backed treatment plans that justify continued therapy sessions.
More consistent reports that align with compliance standards.
Benefits for Patients: Motivation, Engagement, and Measurable Progress
1. Increased Engagement and Adherence
A major barrier to rehabilitation success is lack of motivation. Traditional exercises can feel monotonous, leading to low adherence rates. However, VR therapy transforms exercises into interactive and engaging experiences.
Research Finding:
A narrative review published in Frontiers in Neurology (2024) examined the effectiveness of virtual reality (VR)-based rehabilitation for stroke patients, highlighting its impact on engagement and adherence. The study found that VR therapy significantly increases patient motivation by providing immersive, interactive environments that make rehabilitation exercises more engaging compared to traditional methods. Enhanced engagement leads to higher adherence rates, ultimately improving motor recovery and functional outcomes. The findings support VR’s ability to sustain patient interest while delivering measurable therapeutic benefits, reinforcing its efficacy as a rehabilitation tool (Aderinto et al.)
By making therapy feel like a game, VR keeps patients engaged, leading to better long-term commitment.
2. Personalized Goal Setting
Patients often struggle to see their own progress, which can lead to frustration. VR offers instant feedback, allowing patients to:
Track range of motion improvements.
Monitor reaction time progress.
Receive visual feedback on strength and endurance gains.
3. More Confidence in Their Recovery
When patients see real data on their improvements, they believe in the therapy process.A study published in Frontiers in Psychiatry (2023) examined the effects of virtual reality (VR) therapy on patients with psychosis, highlighting its role in building patient confidence during rehabilitation. The research found that VR-based interventions provided a safe, controlled environment where patients could practice real-world interactions, leading to increased self-assurance and reduced anxiety. Participants reported high satisfaction levels, with many expressing greater confidence in their ability to navigate daily activities after VR therapy. These findings support VR as an effective tool for enhancing self-efficacy while minimizing traditional therapy barriers
VR-Enhanced Rehabilitation Outcomes Across Different Conditions
Stroke Rehabilitation
Stroke survivors often experience impairments in motor function, coordination, and daily living skills. Conventional rehabilitation methods, while effective, sometimes fall short in providing patients with the necessary level of engagement and adaptability. VR-based stroke rehabilitation is proving to be a game-changer by integrating interactive, gamified exercises that mimic real-world tasks.
Research Finding:
A review published in Journal of NeuroEngineering and Rehabilitation (2020) explored the clinical applications of virtual reality (VR) for upper limb motor rehabilitation in stroke patients, emphasizing its effectiveness in enhancing motor function and patient engagement. The study found that VR-based rehabilitation provides task-oriented, interactive exercises that promote neuroplasticity and motor recovery more effectively than traditional therapy. Additionally, VR enables precise tracking of movement patterns, allowing clinicians to monitor patient progress in real-time and adjust therapy accordingly. The evidence supports VR as a clinically validated tool for improving upper limb function and optimizing rehabilitation outcomes. (Kim)
Gait Training in Neurological Disorders
For individuals with neurological disorders such as Parkinson’s disease, multiple sclerosis, or spinal cord injuries, maintaining balance and coordination is a significant challenge. Traditional gait training often involves static environments and limited sensory feedback, which may not be sufficient to improve real-world walking abilities.
Research Finding:
A systematic review published in Frontiers in Aging Neuroscience (2019) examined the impact of virtual reality (VR) rehabilitation on gait and balance in patients with Parkinson’s disease, highlighting its effectiveness in improving mobility and reducing fall risk. The study found that VR-based training enhances motor learning by providing real-time feedback and engaging environments, which help patients practice balance control and walking adaptability in a safe setting. Additionally, participants showed greater confidence in their movements, leading to increased independence in daily activities. These findings support VR as a valuable tool for gait rehabilitation, offering both physical and psychological benefits for Parkinson’s patients ((Lei et al.))
Pain Management in Chronic Conditions
Chronic pain—whether musculoskeletal, neuropathic, or post-surgical—can significantly reduce quality of life and mobility. Many patients rely on medication to manage their symptoms, but VR is emerging as a non-pharmacological alternative for pain relief.
Research Finding:
A study protocol published in JMIR Research Protocols (2024) explores the effectiveness of virtual reality (VR) in reducing perceived pain and anxiety among hospitalized patients, emphasizing its potential as a non-pharmacological intervention. The research aims to evaluate how immersive VR environments provide distraction and relaxation, leading to lower pain perception and reduced anxiety levels during medical treatments. Early findings suggest that VR therapy enhances patient comfort and emotional well-being, making it a promising tool for improving the overall hospital experience. (Mittal et al.)
VR therapy also provides long-term benefits by helping patients develop coping mechanisms, improve mobility, and reduce reliance on pain medications. Patients who engage in VR-based relaxation and cognitive behavioral therapy exercises report higher pain tolerance and reduced anxiety, which play a crucial role in long-term pain management strategies.
Conclusion
Tracking patient outcomes with VR and AI is revolutionizing rehabilitation by providing real-time insights, personalized therapy, and objective progress tracking. The combination of VR-based monitoring and AI-driven documentation is reducing administrative burdens for therapists while keeping patients engaged and motivated.
With an ever-growing body of research supporting VR’s effectiveness in tracking and enhancing patient outcomes, its integration into rehabilitation practices is only expected to expand. The future of rehab is data-driven, engaging, and more precise than ever.
-
Aderinto, Nicholas, et al. “Exploring the Efficacy of Virtual Reality-Based Rehabilitation in Stroke: A Narrative Review of Current Evidence.” Annals of Medicine, vol. 55, no. 2, 27 Nov. 2023, https://doi.org/10.1080/07853890.2023.2285907.
Freeman, Daniel, et al. “Virtual Reality (VR) Therapy for Patients with Psychosis: Satisfaction and Side Effects.” Psychological Medicine, vol. 53, no. 10, 28 Apr. 2022, pp. 1–12, https://doi.org/10.1017/s0033291722001167.
Khan, Ammar, et al. “Virtual Reality in Stroke Recovery: A Meta-Review of Systematic Reviews.” Bioelectronic Medicine, vol. 10, no. 1, 5 Oct. 2024, https://doi.org/10.1186/s42234-024-00150-9.
Kim, Won-Seok . “Clinical Application of Virtual Reality for Upper Limb Motor Rehabilitation in Stroke: Review of Technologies and Clinical Evidence.” Nih.gov, 2025, pmc.ncbi.nlm.nih.gov/articles/PMC7590210/. Accessed 24 Feb. 2025.
Lei, Cheng, et al. “Effects of Virtual Reality Rehabilitation Training on Gait and Balance in Patients with Parkinson’s Disease: A Systematic Review.” PLOS ONE, vol. 14, no. 11, 7 Nov. 2019, p. e0224819, https://doi.org/10.1371/journal.pone.0224819. Accessed 27 Mar. 2020.
Mittal, Ajay, et al. “Effectiveness of Virtual Reality in Reducing Perceived Pain and Anxiety among Patients within a Hospital System: Protocol for a Mixed Methods Study.” JMIR Research Protocols, vol. 13, 9 May 2024, p. e52649, www.ncbi.nlm.nih.gov/pmc/articles/PMC11117134/, https://doi.org/10.2196/52649. Accessed 17 June 2024.
Sumner, Jennifer, et al. “Artificial Intelligence in Physical Rehabilitation: A Systematic Review.” Artificial Intelligence in Medicine, vol. 146, 1 Dec. 2023, p. 102693, www.sciencedirect.com/science/article/pii/S0933365723002075, https://doi.org/10.1016/j.artmed.2023.102693.