From Fear to Hope: First Step for VR Therapy
Written by: Brianna Hodge
Imagine this: You walk into a rehab clinic for your first session. You’re not quite sure what to expect, maybe some stretching, maybe a few weights. But instead, someone hands you a sleek VR headset and says, “We’re going to start with a forest walk today.” Suddenly, you're not in a sterile room anymore. You're surrounded by trees, winding trails, and the gentle sounds of birds overhead. The tension in your shoulders begins to ease, not because of any treatment yet, but because something is different. This feels… hopeful.
This is what virtual reality (VR) therapy can do. It changes the emotional and psychological experience of rehabilitation. But for many first-time patients, the idea of using VR for therapy can be intimidating. They may ask:
Will I understand how to use it?
Will it feel weird?
What if I’m not tech-savvy?
These are normal concerns, and if you’re a clinician introducing VR, or a patient about to try it, it’s important to know how to break the ice gently.
Let’s walk through how we can make that first VR therapy session feel less like stepping into the unknown and more like stepping into a new kind of empowerment.
Why the First Session Matters So Much
The first interaction a patient has with their therapist and the treatment environment really sets the tone for everything that follows. In fact, research from the Psychotherapy and Therapeutic Relationship guide shows that how safe, seen, and supported someone feels in that first session can have a huge impact on how engaged they are and what kind of results they get (Opland and Torrico).
That’s why this moment is so important when you’re introducing something new, like virtual reality. If the headset is handed over without explanation, or the experience feels too high-tech too fast, patients might pull back. But when a therapist takes a few extra minutes to connect, explain, and guide the patient into the experience with care, it makes all the difference. Suddenly, VR doesn’t feel so intimidating, it feels like an exciting new part of the journey you’re taking together.
Understanding the Hesitation: A Real Look at First-Time Anxiety
In my experience, that very first session, the first few minutes, even, can make or break how a patient feels about their entire therapy journey. And when it comes to introducing something unfamiliar like VR, that initial connection matters even more. I truly believe that if a patient doesn’t feel safe, understood, or supported right from the start, it’s going to be tough for them to fully engage, no matter how impressive the technology is.
Imagine this: You’re a patient walking into a clinic for the first time. You’re a little anxious, unsure of what to expect. Instead of the usual exercise equipment, someone hands you a headset and says, “We’ll be using VR today.” Your mind races—What if I can’t figure it out? Will I look silly? Is this even going to help me? Now, imagine instead that the therapist sits beside you, smiles, and says, “You don’t have to do anything yet. Let’s walk through it together.” They show you the headset, let you feel it in your hands, explain what you’ll see, and reassure you that you’re in control the entire time. Suddenly, it doesn’t feel so intimidating. It feels human. Safe. Collaborative.
As we discussed in the last paragraph, those early impressions can have a lasting effect on patient engagement and outcomes. That’s why I’m a big advocate for slowing things down in the beginning, taking the time to explain what VR is, letting patients ask questions, and making it feel approachable. When we treat that first moment like the start of a partnership rather than just a procedure, we open the door to real trust, and that’s where the magic of VR therapy really begins.
Dallas VA
How a Therapist could Ease a Veteran’s First VR Session
Take Michael, for example—a 68-year-old veteran who walked into his physical therapy session with a noticeable limp and an even more noticeable skepticism. He’d been through years of treatment for chronic pain in his back and knees. When he saw the VR headset sitting on the counter, he raised an eyebrow. “I’m not here to play video games,” he muttered.
But his therapist, Lisa, didn’t rush. She smiled and responded warmly, “That’s fair. But this isn’t gaming—it’s therapy that just happens to take place in a really engaging way. You don’t have to commit to anything today. I’d just love to show you how it works.”
Instead of putting the headset on him right away, Lisa let Michael hold it. She explained how it worked, and that everything would move at his pace. She pulled up a calming ocean scene and said, “Would it be okay if I placed it on you just so you can take a look? We don’t have to do anything else.”
Michael hesitated, but agreed. A few moments into the experience, he whispered, “This reminds me of the beach in Coronado. I haven’t felt this relaxed in months.”
They didn’t do any formal therapy that day. Lisa just let him explore. But that small moment, no pressure, just support, built the trust they needed. By the next session, Michael was ready to try gentle movements while in VR. Three weeks later, he was completing guided trunk rotations in a virtual forest, and reporting less pain and more motivation than he’d felt in years.
Setting the Stage: How to Prepare the Room and the Mind
Introducing VR therapy successfully starts before the headset even comes out of its case. Here’s how you can create the right conditions:
1. Start with Conversation, Not Tech
Begin by asking about the patient’s comfort with technology. This small gesture does more than gather information, it shows empathy. It tells the patient, “I see you, and I want to meet you where you are.” Some people might light up and say, “Oh, I’ve tried VR before!” while others may admit they’ve never even worn a headset. Either way, starting the conversation with curiosity helps build rapport.
Once you’ve opened that door, be sure to reassure them that no prior experience is needed at all. Emphasize that this isn’t something they have to “figure out” or “get right.” You can say something like, “You won’t need any controllers or buttons to start with—we’ll just begin by relaxing in a calm, peaceful environment.” That single sentence alone can lift a weight off someone’s shoulders.
People are often afraid of making mistakes, especially when something feels foreign. By framing the session as a chance to experience rather than perform, you take away the pressure. Let them know they can stop at any time, that they’ll be guided the whole way, and that their comfort is the priority. This approach not only builds trust, it lays the groundwork for meaningful engagement right from the very first session.
2. Introduce the Hardware Gently
Let them hold the headset first. Give them a moment to feel its weight, examine the lenses, and understand that it’s not as intimidating as it might seem. Encourage them to look inside—point out how it’s just a screen, not much different than a phone or tablet, only more immersive. Then, gently guide them to try it on while it’s still turned off. No visuals, no sounds, just the sensation of wearing it.
This small, seemingly simple step goes a long way. It removes the element of surprise and allows the patient to adjust to how the headset feels on their head and face. Desensitization like this can significantly reduce initial resistance because it gives the patient a sense of control. They get to experience it on their terms, without pressure. For someone who’s already navigating pain, anxiety, or unfamiliar environments, that control can make all the difference in whether they open up to the experience, or shut down before it even begins.
3. Use Familiar, Calming Environments First
In my opinion, the best way to ease someone into their first VR session is by starting with a calming, natural environment. There's something inherently comforting about walking through a forest path, listening to gentle waves on a beach, or sitting in a peaceful garden, even if it’s virtual.
I’ve found that these types of scenes help people relax, feel less overwhelmed, and start to enjoy the experience without worrying about doing anything “right.” Jumping straight into a fast-paced or game-like simulation can be too much too soon, especially if someone’s already anxious about trying something new. Starting slow, with something serene, can really change everything.
The Power of Presence: Why VR Feels So Real
What makes VR so different from watching a video on a screen? It’s the feeling of presence—the sense that you are physically “in” the environment.
Research:
One of the most fascinating aspects of VR therapy is how the brain responds to it. Neuroscience has shown that immersive virtual environments can activate many of the same neural circuits involved in real-life experiences.
According to the review Neuroscience of Virtual Reality: From Virtual Exposure to Embodied Medicine, when individuals engage in VR tasks, areas of the brain responsible for perception, motor planning, and emotional processing light up just as they would if the person were physically present in that environment (Riva et al.).
This phenomenon is partly due to what’s known as embodied simulation, where the brain interprets virtual actions as though they are happening in the real world. That’s why patients practicing balance, motor control, or even pain management in VR often show measurable improvements, it’s not just pretend play; it’s real neural engagement. For therapists and patients alike, this means that VR isn’t just a fun distraction, it’s a tool that leverages the brain’s natural wiring to support meaningful, functional change.
This presence creates emotional and physiological engagement. When patients are immersed in VR, they are more likely to stay focused, tolerate discomfort, and even forget they are doing therapy. That’s not just anecdotal—that’s supported by neuroimaging and behavioral research
Neuroplasticity Starts with Engagement
One of the most promising aspects of VR therapy is its impact on neuroplasticity—the brain’s ability to reorganize itself by forming new neural connections. But neuroplasticity doesn’t happen by chance. It requires attention, repetition, and challenge.
Research:
When it comes to stroke rehabilitation, especially for upper-limb recovery, cognitive engagement is a game-changer, and that’s where VR stands out. According to the narrative review Exploring the Efficacy of Virtual Reality-Based Rehabilitation in Stroke, stroke patients who participated in VR-based upper-limb therapy consistently demonstrated greater improvements in motor function compared to those undergoing traditional rehabilitation methods (Aderinto et al.).
What makes the difference? It’s the immersive, interactive nature of VR. Unlike repetitive, passive exercises, VR demands attention, decision-making, and real-time feedback, all of which stimulate cognitive processes that are critical for neuroplasticity and functional recovery. This heightened mental involvement keeps patients motivated and emotionally invested, ultimately leading to more consistent participation and better outcomes. In other words, VR doesn't just move the body—it activates the brain.
In other words, patients weren’t just doing the exercises, they were immersed in them.
Breaking the Ice with Pediatric Patients
One of the most underrated superpowers of VR is its ability to turn therapy into something that feels like play, especially for kids. Traditional therapy for children with cerebral palsy or traumatic brain injury can be repetitive, exhausting, and potentially boring for children. That’s a tough ask for a child who’s already navigating so many challenges. But VR changes the entire tone. I’ve seen how quickly kids go from resistant to engaged the moment they step into a virtual world where therapy feels like an adventure.
And it’s not just anecdotal. A study published in Virtual Reality for Distraction and Relaxation in a Pediatric Hospital Setting found that VR significantly reduced distress and boosted positive emotions in pediatric patients, even in stressful hospital environments (Bernaerts et al.). When therapy is low-pressure, fun, and immersive, it opens the door for more consistent participation—and that’s when real progress starts to happen. I fully believe that when used thoughtfully, VR can be the key to unlocking a child’s willingness to engage in their own healing.
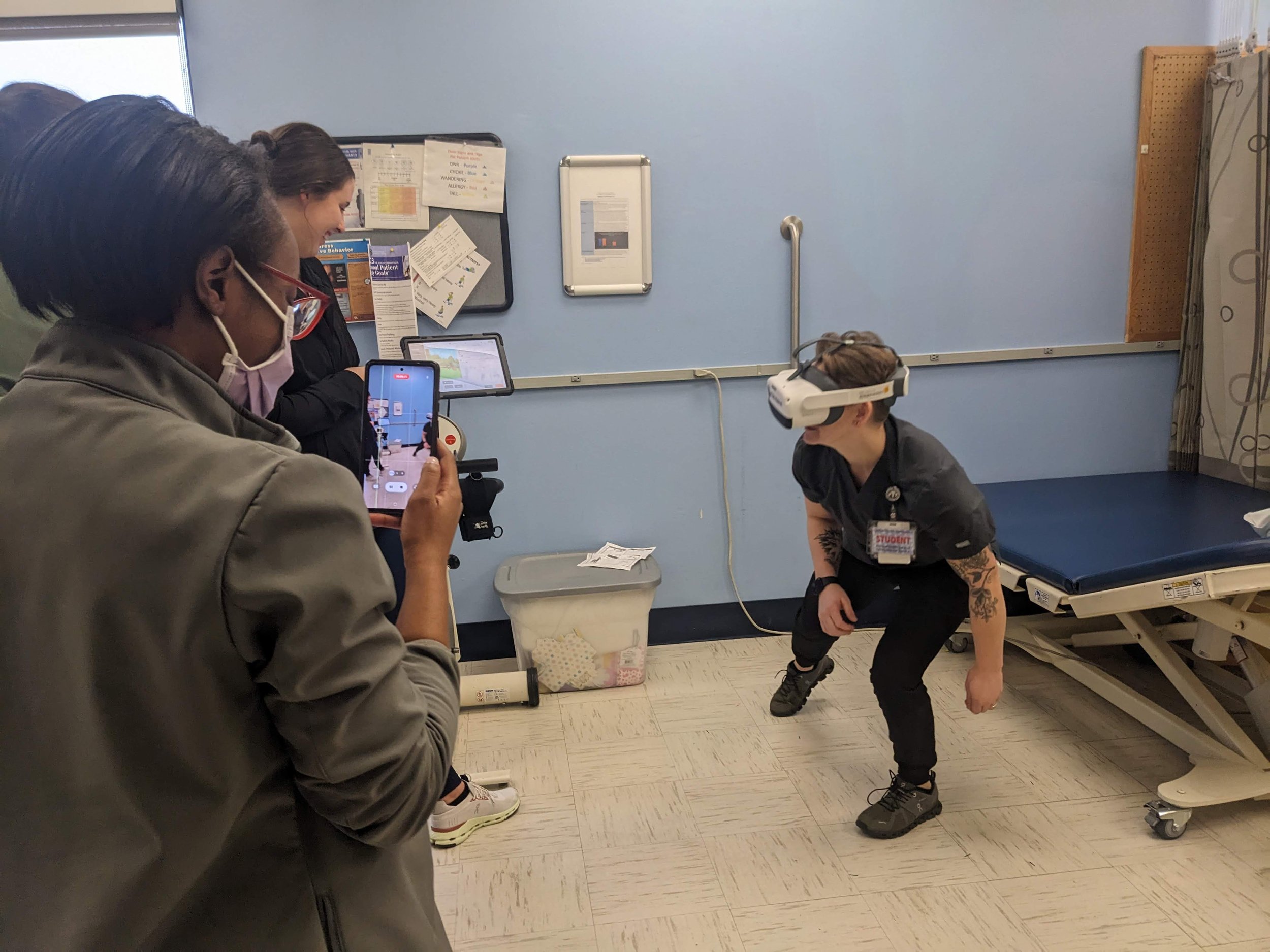
The Role of the Clinician as a VR Guide
Clinicians don’t need to be tech experts—they need to be experienced guides. Their true value lies in how they support the patient’s journey, not in mastering every button or software update. It’s their role to monitor emotional and physical responses, adjust the difficulty in real time, and reinforce every bit of progress. VR therapy is most effective when it’s paired with real human connection, and that’s where clinicians shine.
During those early sessions, it’s crucial to stay close, offer steady verbal encouragement, and take time to debrief afterward. Ask questions like, “How did that feel?” “Was anything confusing?” or “Did you enjoy that experience?” These check-ins not only help guide the next session, they build trust and lay the foundation for continued use.
For therapists who want to feel more confident introducing this technology, Neuro Rehab VR even offers a CEU-certified course designed to walk clinicians through everything they need to know, from setup to patient engagement strategies. It’s not about becoming a tech guru. It’s about learning how to create meaningful, healing experiences through VR.
Introducing VR to Elderly Patients
One of the most encouraging things I’ve seen, and that research supports, is how older adults respond to VR therapy once they’ve actually experienced it. There’s often hesitation at first, especially from patients over 70, but that initial skepticism tends to disappear quickly.
Research:
According to the systematic review Effectiveness of Virtual Reality Therapy on Balance and Gait in the Elderly, the majority of older participants reported overwhelmingly positive reactions after trying VR, with many even saying they preferred it to traditional therapy methods (Rodríguez-Almagro et al.).
These are individuals who may have limited mobility, chronic balance issues, or a fear of falling—and yet, they’re choosing VR because it feels safer, more engaging, and even enjoyable. It goes to show that age isn’t a barrier to innovation.
With the right introduction and support, VR can be just as transformative for seniors as it is for younger patients.
The key? Go slow. Allow more time for acclimation. Choose low-stimulation content initially. Emphasize benefits they care about: reduced pain, better mobility, improved confidence.
Neuro Rehab VR’s Approach to First-Time Patients
At Neuro Rehab VR, introducing first-time patients to VR isn’t just a feature, it’s a philosophy. Whether in skilled nursing facilities, hospitals, or outpatient clinics, the approach is centered around empowerment through simplicity.
Patients start with environments that are familiar and calming, like walking down a trail or being placed in a serene environment.
Therapists can personalize sessions in real-time using a clinician tablet, which allows on-the-fly adjustments to difficulty and intensity. Perhaps most importantly, the team at Neuro Rehab VR trains clinicians not just on the how of using the system, but on the why of patient-first, confidence-building experiences.
One therapist shared this quote after introducing a patient with Parkinson’s to the system: “He was hesitant at first, but within five minutes, he was laughing. He said it was the first time in months he forgot about his tremors.”
That’s not just therapy. That’s transformation.
Key Strategies for Clinicians
Let’s recap some practical strategies that clinicians can use to break the ice for VR-first-timers:
Start with curiosity. Ask about tech comfort, past experience, and emotional readiness.
Keep it low pressure. Let patients watch before participating. Give them control.
Pick calming environments. Avoid overstimulation during early sessions.
Narrate the process. Tell them what to expect before they experience it.
Debrief afterward. Use open-ended questions to guide reflection.
Celebrate micro-wins. Small achievements in VR often feel big to patients.
Final Thoughts: The First Step Changes Everything
Introducing VR therapy to someone for the first time is like opening a door to a new way of healing. That first moment of surprise, that first smile or sigh of relief—it matters. It’s the beginning of a relationship between technology, the brain, and the person who is rebuilding their strength.
And while the science is strong, the human connection is stronger. When done thoughtfully, VR doesn’t replace the therapist, it amplifies their impact.
So if you’re a clinician reading this: The next time you put a headset in someone’s hands, remember you’re not just giving them a tool. You’re giving them hope.
And if you’re a patient about to try VR therapy for the first time: You don’t have to know everything. You just have to take that first, brave step.
-
Aderinto, Nicholas, et al. “Exploring the Efficacy of Virtual Reality-Based Rehabilitation in Stroke: A Narrative Review of Current Evidence.” Annals of Medicine, vol. 55, no. 2, 27 Nov. 2023, https://doi.org/10.1080/07853890.2023.2285907.
Bernaerts, Sylvie, et al. “Virtual Reality for Distraction and Relaxation in a Pediatric Hospital Setting: An Interventional Study with a Mixed-Methods Design.” Frontiers in Digital Health, vol. 4, 31 May 2022, https://doi.org/10.3389/fdgth.2022.866119.
Opland, Caitlin, and Tyler J Torrico. “Psychotherapy and Therapeutic Relationship.” Nih.gov, StatPearls Publishing, 2024, www.ncbi.nlm.nih.gov/books/NBK608012/.
Riva, Giuseppe, et al. “Neuroscience of Virtual Reality: From Virtual Exposure to Embodied Medicine.” Cyberpsychology, Behavior and Social Networking, vol. 22, no. 1, 1 Jan. 2019, pp. 82–96, www.ncbi.nlm.nih.gov/pmc/articles/PMC6354552/, https://doi.org/10.1089/cyber.2017.29099.gri.
Rodríguez-Almagro, Daniel, et al. “Effectiveness of Virtual Reality Therapy on Balance and Gait in the Elderly: A Systematic Review.” Healthcare, vol. 12, no. 2, 9 Jan. 2024, pp. 158–158, doi.org/10.3390%2Fhealthcare12020158, https://doi.org/10.3390/healthcare12020158.