From Classroom to Clinic: Dynamic Rehab Training using VR
Written by: Brianna Hodge
If you’re leading a physical therapy or occupational therapy program today, you know the stakes are higher than ever. Your students are entering a healthcare environment that is more complex, data-driven, and technology-dependent than at any time in history. Patient populations are more diverse. Clinical settings are more fast-paced. And the tools of care, from robotics to AI-assisted charting, are advancing faster than traditional curriculums can adapt.
That’s why simply preparing students with textbooks, mannequin labs, and role-play scenarios is no longer enough. The next generation of rehab professionals must not only master anatomy and technique, they must also develop the agility to work seamlessly with emerging technologies, adapt to rapidly changing conditions, and engage patients in meaningful, personalized ways.
Artificial intelligence (AI) and virtual reality (VR) simulation labs are no longer futuristic “add-ons.” They’re becoming the bridge between theory and practice, the immersive environments where students can safely make mistakes, learn from them instantly, and carry that confidence into real patient care.
Rowan-Cabarrus Community College
How VR can enhance Traditional Labs
Mannequin-based labs and peer role-play have been the backbone of rehab training for decades. These methods are familiar, relatively low-cost, and can be effective for teaching certain foundational skills. But they have limitations, especially when compared to the demands of today’s clinical environments.
Static scenarios – A mannequin can’t adapt its responses, simulate complex emotions, or mimic the unpredictable nature of real patient presentations.
Limited repetition – Setting up physical labs for complex scenarios can be time-consuming, limiting the number of practice opportunities for students.
Minimal exposure to rare cases – Students may graduate without ever practicing responses to uncommon but critical clinical situations.
Feedback delays – Faculty can’t be everywhere at once, and immediate, detailed feedback is hard to provide in traditional labs.
How VR Overcomes These Challenges:
Dynamic patient responses – Unlike mannequins, VR patients can move, speak, and react with realistic physical and emotional behaviors, preparing students for real-world unpredictability.
Unlimited practice – Complex scenarios can be launched instantly and repeated as often as needed, giving every student more hands-on time without the setup burden of physical labs.
Exposure to rare cases – VR allows educators to design and deploy uncommon but critical clinical situations, ensuring students practice responses they might never encounter during rotations.
Immediate feedback – AI-driven analysis provides students with real-time insights into their performance, covering movement quality, safety, and communication, so they can learn and adjust on the spot.
By shifting from only using traditional labs to adaptive VR environments, you give students the chance to experience training that is more realistic, repeatable, and responsive, building both technical skill and clinical confidence before they ever step into a real patient’s room.
AI and VR Simulation Labs Explained
AI in Rehab Education
Artificial intelligence acts as the silent partner in simulation labs, analyzing student performance in real-time, adapting scenarios, and offering feedback that’s specific, actionable, and personalized. AI systems can track everything from movement accuracy to decision-making speed, helping educators identify gaps that might not be obvious during observation.
VR in Rehab Education
Virtual reality creates the immersive environment where the learning happens. Instead of reading about a stroke patient’s mobility challenges, a student can step into a fully simulated rehab room and guide a virtual patient through exercises, adjusting their approach as the AI tracks outcomes. These environments can replicate outpatient clinics, home health visits, or even high-pressure acute care settings.
When combined, AI and VR create a feedback loop that’s difficult to replicate in any other setting. The AI ensures each session is challenging yet achievable, while VR ensures each session feels as real as possible.
Evidence That AI + VR Improve Rehab Education
The research is clear, students trained with immersive technology consistently demonstrate stronger skills, greater confidence, and improved patient interaction.
Clinical reasoning
A growing body of evidence supports the impact of simulation-based training on healthcare education. In a recent review, researchers found that VR-based clinical simulations significantly improved healthcare students’ diagnostic reasoning and procedural accuracy when compared to traditional teaching methods.
The study emphasized that immersive environments allow learners to apply knowledge in dynamic, realistic contexts, which strengthens both cognitive decision-making and hands-on skills. For PT and OT programs, this means students aren’t just memorizing steps, they’re practicing the critical reasoning and procedural precision they’ll need in clinical placements and beyond. (Elendu et al.)
Skill retention
One of the biggest challenges in rehab education is ensuring that students don’t just perform well during training, but that they retain those skills long after the classroom experience ends. A study on simulation-based mastery learning demonstrated that students who trained in immersive simulation environments showed markedly better long-term retention of complex procedural skills compared to those taught with traditional methods.
This reinforces the value of VR in PT and OT education, not only can students achieve competency faster, but they’re also more likely to carry those skills into clinical practice with confidence and accuracy. (Moazed et al.)
Soft skills and empathy
Beyond technical expertise, successful rehabilitation professionals rely heavily on soft skills, the ability to communicate clearly, build trust, and demonstrate empathy. A protocol review exploring virtual reality for communication training in medical and graduate education highlights that immersive environments can significantly enhance empathy, cultural competence, and interpersonal communication skills.
For PT and OT programs, this means students can practice sensitive conversations, such as motivating patients who feel discouraged or navigating cultural nuances, in a safe, simulated space, better preparing them for the diverse patient populations they will serve. (Khodabakhshian et al.)
For rehab education, where the physical and emotional aspects of care are deeply intertwined, these benefits are game-changing.
The Student Experience in AI + VR Labs
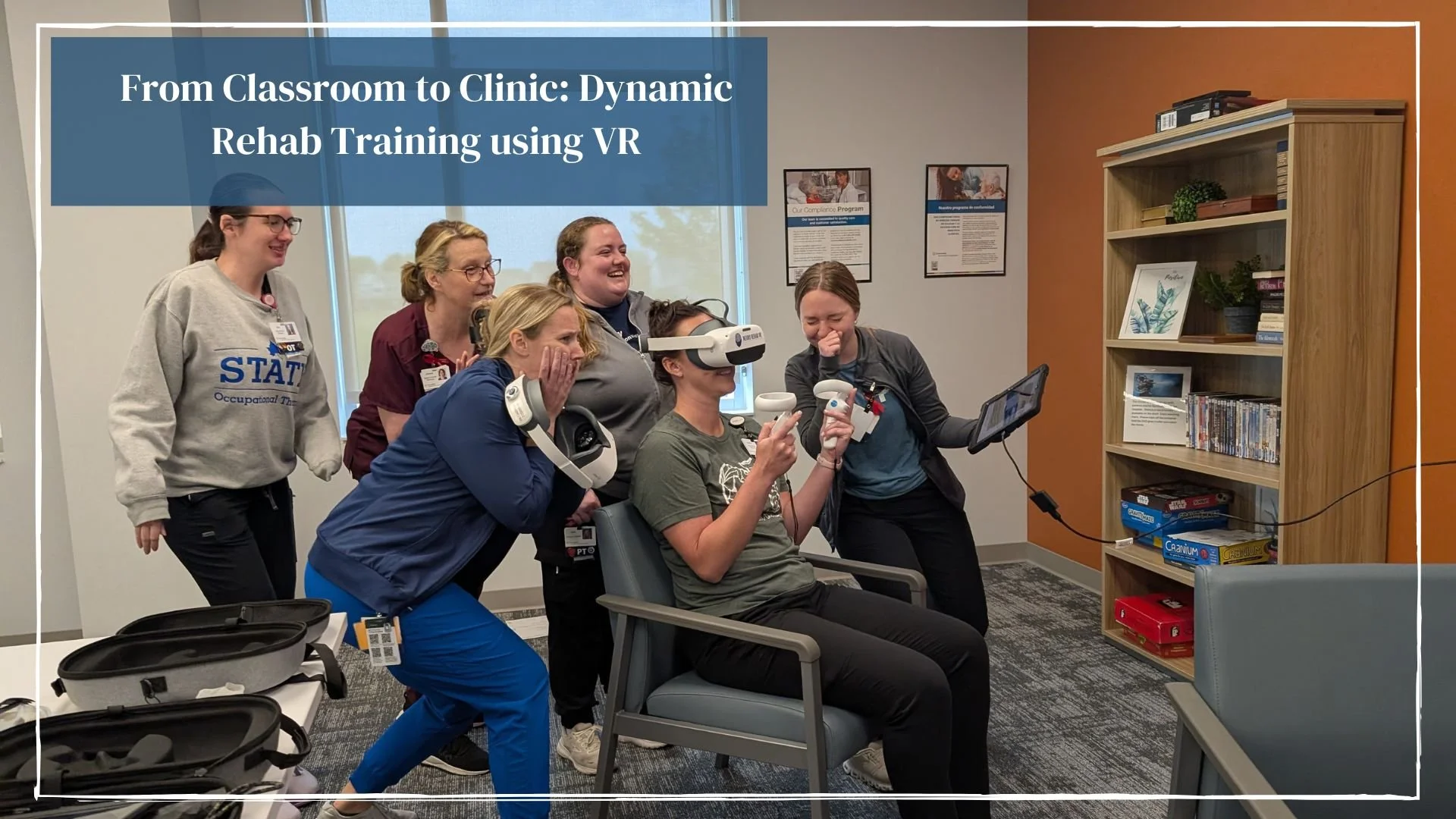
Imagine guiding your students into a simulation lab where they each don a headset and find themselves in a patient’s living room. The “patient,” portrayed through VR, struggles to transfer from a couch to a walker. The student must assess the scene, give instructions, and adjust the plan on the fly when the patient becomes fatigued. AI monitors their tone of voice, body positioning, and safety precautions, then delivers a detailed report for debrief.
In this environment, students learn more than just task completion, they practice clinical reasoning, problem-solving, and patient-centered communication. The stakes feel real, but the setting allows for trial, error, and mastery without risk to actual patients.
Accreditation Alignment: CAPTE and ACOTE Competencies
For program directors, the decision to invest in AI and VR isn’t just about innovation, it’s about accreditation. Both the Commission on Accreditation in Physical Therapy Education (CAPTE) and the Accreditation Council for Occupational Therapy Education (ACOTE) outline competencies that immersive simulation directly supports.
CAPTE-aligned skills:
Patient examination and evaluation – Simulated patients allow for repeated practice in assessment and documentation.
Clinical decision-making – AI-adaptive scenarios challenge students to select interventions based on evolving conditions.
Professional and ethical behavior – Role-play of sensitive situations helps students navigate ethical dilemmas and cultural competency.
ACOTE-aligned skills:
Intervention planning and implementation – VR environments allow for safe, repeatable practice in ADL retraining, mobility work, and environmental modifications.
Therapeutic use of self – Realistic patient avatars help students refine their communication and rapport-building skills.
Evidence-based practice – Data from AI analysis supports integration of research into decision-making.
By directly mapping VR and AI training to these competencies, you’re not just enhancing learning, you’re strengthening your program’s compliance and reputation.
Neuro Rehab VR in Action at Universities
Neuro Rehab VR partners with universities across the country to integrate AI-powered VR rehabilitation tools into their training curriculums. Some of our partners include:
Marshall University School of Physical Therapy
Quinnipiac University Department of Occupational Therapy
Rowan-Cabarrus Community College
University of Dayton
University of Michigan (Sparrow Specialty Hospital)
University of Texas at Arlington
Victoria College
In these programs, students use Neuro Rehab VR’s immersive environments to practice gait training, balance exercises, and ADL scenarios. The AI-driven platform tracks their performance, providing immediate, measurable feedback on metrics like movement accuracy, timing, and patient engagement strategies.
Faculty report that the technology not only boosts student confidence but also allows them to identify skill gaps earlier, making targeted remediation possible before clinical placements.
Beyond Students: Faculty Development Through CEU Courses
Preparing students with immersive technology is only one part of the equation, the other is ensuring that faculty and practicing clinicians feel confident and empowered to use it. That’s why Neuro Rehab VR also offers continuing education (CEU) courses designed specifically for rehabilitation professionals. These courses provide foundational knowledge in virtual reality therapy, demonstrate best practices for integration, and highlight how AI-driven insights can streamline clinical documentation and enhance patient care.
For universities, CEU offerings serve as an important bridge. Faculty can gain hands-on experience in VR environments while earning credits toward their professional development requirements. This not only strengthens instructors’ confidence in bringing VR into the classroom but also ensures that your program maintains a reputation for innovation and academic excellence. By investing in both students and educators, your institution builds a sustainable model where immersive technology is not a novelty but a core part of training the next generation.
How These Labs Prepare Students for Day 1 in the Clinic
Graduates trained with AI and VR enter the workforce with a noticeable edge. Instead of encountering complex cases for the very first time during clinical rotations, they’ve already practiced them in a safe, immersive lab. They’re accustomed to thinking critically in dynamic environments, adapting their interventions in real time as conditions change, and reflecting immediately on their own performance with the help of AI-driven feedback.
These experiences significantly reduce the “transition shock” that many new clinicians feel when stepping from the classroom into patient care. Instead of hesitation, they approach their first patients with confidence, having rehearsed everything from high-stakes emergency responses to delicate patient communication. This translates into faster decision-making, safer interventions, and a stronger ability to build trust with patients.
For educators, the difference is clear: students who train with immersive tools don’t just graduate with theoretical knowledge, they leave with the clinical readiness, adaptability, and resilience to thrive from day one. And in a healthcare system that demands efficiency, empathy, and evidence-based practice, those are the qualities that set your graduates, and your program, apart.
Addressing Faculty Concerns
It’s natural for faculty and administrators to have questions before adopting new technology. Shifting from traditional labs to AI- and VR-based training can feel like a significant change, but the reality is that many of the common concerns can be addressed with thoughtful planning and the right partner.
Cost
While immersive technology does require an upfront investment, its long-term value often exceeds that of traditional lab equipment. Once purchased, VR scenarios can be reused across multiple cohorts, eliminating the need for constant replacement or reset of physical training materials. In addition, because sessions can be repeated indefinitely, students gain more practice without driving up costs. The scalability of these systems means you can train an entire class simultaneously, rather than relying on faculty-intensive small group setups. Over time, the savings in equipment, space, and staff resources can make VR not only cost-effective but cost-saving.
Faculty Training
Another common hesitation is whether instructors will feel confident enough to guide students in virtual environments. This is where Neuro Rehab VR places a strong emphasis on support. Every partner institution receives onboarding that’s tailored to their program, ensuring faculty have hands-on experience with the system before introducing it to students. Beyond onboarding, continuous support and updates are available so faculty never feel like they are navigating the technology alone. This ongoing relationship helps transform VR from something new and intimidating into an accessible, reliable teaching tool.
Curriculum Integration
The fear of disruption is also common—many educators wonder if adopting VR means overhauling their entire curriculum. The reality is quite the opposite. Simulation modules can be aligned seamlessly with existing coursework, serving as an enhancement rather than a replacement. For example, a neurorehabilitation lecture can be followed by a VR-based gait training lab, giving students a chance to apply concepts immediately. Faculty maintain full control over when and how to deploy scenarios, making the technology flexible and adaptable to each program’s specific learning outcomes and accreditation requirements.
When these concerns are addressed head-on, the path forward becomes clear: AI- and VR-based simulation is not an obstacle to overcome, but an opportunity to elevate faculty teaching, optimize resources, and enhance student readiness.
Your Next Step – Bringing the Future to Your Program
The next generation of PTs and OTs will practice in a healthcare landscape where AI, VR, robotics, and data-driven systems are not optional—they’re essential. Clinics and hospitals are already adopting immersive technologies to train staff, improve patient outcomes, and streamline workflows. By integrating AI and VR simulation labs into your program today, you ensure your students are not left behind. Instead, they gain the opportunity to practice, fail, learn, and ultimately succeed in a safe yet highly realistic environment.
This isn’t just about giving students access to new technology—it’s about transforming the way they learn. Immersive labs provide students with repeated exposure to rare cases, opportunities to develop empathy and cultural competence, and immediate feedback that strengthens both clinical skills and confidence. When your graduates walk into their first day of clinical practice, they won’t be encountering these challenges for the first time—they’ll already have the mindset and experience of a seasoned professional.
Neuro Rehab VR is here to help your program make that leap. With a proven track record of partnerships at leading universities, a curriculum that aligns with CAPTE and ACOTE standards, and ongoing support for faculty, Neuro Rehab VR provides more than just technology—it provides a roadmap for preparing graduates to not only enter the profession but to shape its future. By taking this step now, you’re signaling to students, faculty, and the broader healthcare community that your institution is committed to innovation, excellence, and leadership in rehabilitation education.
-
Elendu, Chukwuka, et al. “The Impact of Simulation-Based Training in Medical Education: A Review.” Medicine, vol. 103, no. 27, 5 July 2024, pp. 1–14, journals.lww.com/md-journal/fulltext/2024/07050/the_impact_of_simulation_based_training_in_medical.22.aspx, https://doi.org/10.1097/MD.0000000000038813.
Khodabakhshian, Nairy, et al. “Virtual Reality for Developing Patient-Facing Communication Skills in Medical and Graduate Education: Protocol for a Scoping Review.” JMIR Research Protocols, vol. 13, 1 Feb. 2024, p. e53901, pubmed.ncbi.nlm.nih.gov/38300671/, https://doi.org/10.2196/53901.
Moazed, Farzad, et al. “Retention of Critical Care Skills after Simulation-Based Mastery Learning.” Journal of Graduate Medical Education, vol. 5, no. 3, 1 Sept. 2013, pp. 458–463, https://doi.org/10.4300/jgme-d-13-00033.1. Accessed 6 Mar. 2021.