Step Into Recovery with VR:Gait Training After Injury
Written by: Brianna Hodge
If you've ever sprained your ankle, had surgery, or just felt unsteady walking after a long illness, you understand that something as "simple" as walking is incredibly complex. Now imagine trying to relearn that skill after a stroke, a spinal cord injury, or years of mobility challenges. It’s not just about physical strength, it’s about balance, coordination, confidence, and your brain's ability to communicate with your body. And that’s where virtual reality (VR) steps in.
In this blog, we’re going to explore how VR is revolutionizing lower-limb and gait training. Whether you're a patient, a therapist, or someone curious about the future of rehab, this isn't just about flashy headsets or digital worlds. It’s about real people reclaiming their independence, one virtual step at a time.
Rowan-Cabarrus Community College
Why Lower-Limb Rehabilitation Matters
Lower-limb mobility is essential to everyday life. From walking across the room to stepping into the shower, standing at the kitchen sink, or climbing stairs, our legs are our primary tools for independence. When injury or illness affects this system, the ripple effects touch every corner of life: physical health declines, mental health suffers, and social isolation can deepen.
Traditional physical therapy, such as; treadmill walking, step-ups, weight-shifting exercises, has always played a vital role in recovery. But it can be repetitive, intimidating, and even discouraging. And that’s where the immersive, adaptive nature of VR changes the game.
What Makes VR Effective for Gait and Lower-Limb Therapy?
At its core, VR offers something powerful: engagement. Instead of focusing on the pain, fatigue, or frustration of rehab, VR redirects attention toward the task at hand. Such as navigating a virtual garden path, crossing a busy city street, or stepping over obstacles in a forest. These environments aren’t just fun, they activate the brain’s reward centers and mimic real-world challenges in a safe, controlled space.
Several key components make VR so uniquely suited for lower-limb rehab:
Multisensory Feedback – Visual cues, sound effects, and haptic feedback enhance body awareness and coordination.
Real-Time Correction – Immediate feedback allows patients to adjust their gait, posture, and step length on the fly.
Motivation & Gamification – Rehab becomes a game, increasing adherence and enjoyment.
Customizable Difficulty – Tasks can be tailored to each patient’s ability and progressed as they improve.
Safe Simulation – Environments like stairs or uneven terrain can be practiced without risk of falls.
What the Research Says: Evidence-Based Practice
If you’re skeptical, you’re not alone. Any new technology in healthcare needs to prove itself. Fortunately, a growing body of research supports VR’s effectiveness for gait and lower-limb training.
VR Improves Gait After Stroke
Research:
Virtual reality has shown significant promise in improving gait function after stroke by offering an engaging, task-specific, and feedback-rich environment. According to a review titled “Virtual reality for stroke rehabilitation”, VR interventions can enhance motor recovery by promoting neuroplasticity through repetitive, goal-directed movement patterns that mimic real-world walking tasks.
In stroke survivors, impaired gait is often linked not just to muscular weakness but also to disrupted neural pathways. VR-based therapy addresses both by combining visual and auditory feedback with interactive scenarios that stimulate sensorimotor integration. The study highlights that patients undergoing VR gait training demonstrated improvements in walking speed, balance, and symmetry, particularly when programs were personalized and incorporated real-time feedback.
These gains suggest that VR can serve as a valuable adjunct to conventional therapy, helping stroke patients regain mobility and confidence in a more motivating and immersive way. (Laver et al.)
VR Enhances Balance in Elderly Populations
Research:
Immersive virtual reality (VR) is proving to be a valuable tool in fall prevention by enhancing balance and walking stability in older adults. VR environments that simulate the affective and physical challenges of everyday situations—like navigating crowded sidewalks or stepping over uneven surfaces—can train users to respond more confidently and safely in the real world.
In their study, participants engaged in immersive VR tasks requiring real-time balance adjustments and obstacle negotiation. This exposure led to measurable improvements in dynamic balance, postural control, and gait stability.
By mimicking realistic environments, VR not only challenges physical capabilities but also addresses the emotional context of fear of falling—creating a more holistic and effective training experience that supports real-world mobility and safety in aging populations.(Raffegeau et al.)
Pediatric Cerebral Palsy and VR
Research:
For children with cerebral palsy, combining treadmill training with virtual reality (VR) has demonstrated remarkable improvements in functional mobility. In a randomized clinical trial titled “Effectiveness of virtual reality on functional mobility during treadmill training in children with cerebral palsy: a single-blind, two-arm parallel group randomised clinical trial“, participants who engaged in VR-enhanced treadmill sessions showed significantly greater gains in gait, balance, and lower-limb muscle strength compared to those who received treadmill training alone.
Beyond the physical improvements, the study also reported increased motivation, engagement, and adherence among children in the VR group. By transforming repetitive exercises into interactive and goal-oriented activities, VR helped reduce boredom and fatigue—two common barriers in pediatric rehabilitation.
These findings highlight VR's potential not only as a powerful motor training tool but also as a means to make therapy more enjoyable and sustainable for young patients. (Ochandorena-Acha et al.)
The Neuroplasticity Link: Training the Brain, Not Just the Body
Gait rehabilitation isn’t just about retraining muscles—it’s about rewiring the brain. Virtual reality taps into the brain’s natural capacity for neuroplasticity: the ability to form new neural connections in response to experience.
When a patient moves through a virtual environment, their brain engages in motor planning, spatial awareness, and visual processing—all while receiving real-time feedback on their movements. This full-brain involvement strengthens neural pathways more effectively than passive or isolated exercises.
Research:
Gait rehabilitation isn’t just about retraining the body, it’s about retraining the brain. Virtual reality harnesses the brain’s natural neuroplasticity, enabling stroke survivors to form new neural connections in response to immersive motor tasks. A study titled “Cerebral Reorganization in Subacute Stroke Survivors after Virtual Reality-Based Training: A Preliminary Study“, found that stroke patients who participated in VR-based gait training showed significant cerebral reorganization, particularly in the premotor cortex and supplementary motor areas. These regions are critical for planning and executing movement.
Unlike passive exercises, VR stimulates the brain through interactive environments that require spatial awareness, motor coordination, and decision-making in real time. This multisensory engagement accelerates the rebuilding of motor pathways and leads to more meaningful, lasting recovery. In essence, VR doesn’t just move the legs, it rewires the mind to move them better (Xiao et al.).
Real-Life Scenario: Imagine This
Imagine you're recovering from a hip fracture. The surgery was successful, but the recovery? That’s a whole different challenge. You’re nervous about putting weight on your leg again. Every movement feels unfamiliar, like your body has forgotten how to walk. You’ve been told to “take it slow,” but even walking down your own hallway feels like standing at the base of a mountain.
You're not just dealing with physical pain - you’re battling fear, hesitation, and the subtle voice in your head that says, What if I fall again?
Now, instead of staring at the cold, tiled floor or counting steps with anxious precision, you slip on a VR headset. Suddenly, the sterile rehab room disappears. You’re standing barefoot on a virtual beach. Warm sunlight glows on the horizon. The waves crash gently in the distance, and a light breeze rustles nearby palm trees. With each step, you follow a trail of footprints imprinted in the soft sand. They’re spaced just right for your current gait, guiding you forward with calm encouragement.
You lift your foot and place it down, not on fear, but on intention. You step again. And again. The unevenness of the sand requires balance. You engage muscles you haven’t used in weeks. But you don’t notice the strain because your mind is elsewhere, focused on the rhythm of the waves, the serenity of the scenery, and the sense of peace that comes from doing something that feels normal again.
Suddenly, you’re not in rehab, you’re on a peaceful walk at the beach.
This is what VR offers: a space where therapy becomes purposeful, immersive, and emotionally supportive. You're no longer just a patient completing a set of exercises. You're a person, moving through an environment that feels real, regaining control of your body in a way that traditional therapy rarely allows.
Customizing Therapy: How VR Adapts to Every Step
One of the most powerful aspects of VR is how adaptive it is. Unlike static exercise programs, VR environments and tasks can change in response to real-time performance.
Some systems use motion capture or pressure sensors to track foot placement, step length, and limb symmetry. AI algorithms then adjust the terrain, speed, or level of challenge. For example, if a patient shows weakness on one side, the VR system might encourage weight-shifting to that side or present a path that promotes more symmetrical gait.
This dynamic feedback loop ensures that therapy remains effective without overwhelming the patient—something traditional therapy often struggles to do in real time.
Section: Neuro Rehab VR—Smart Therapy in Action
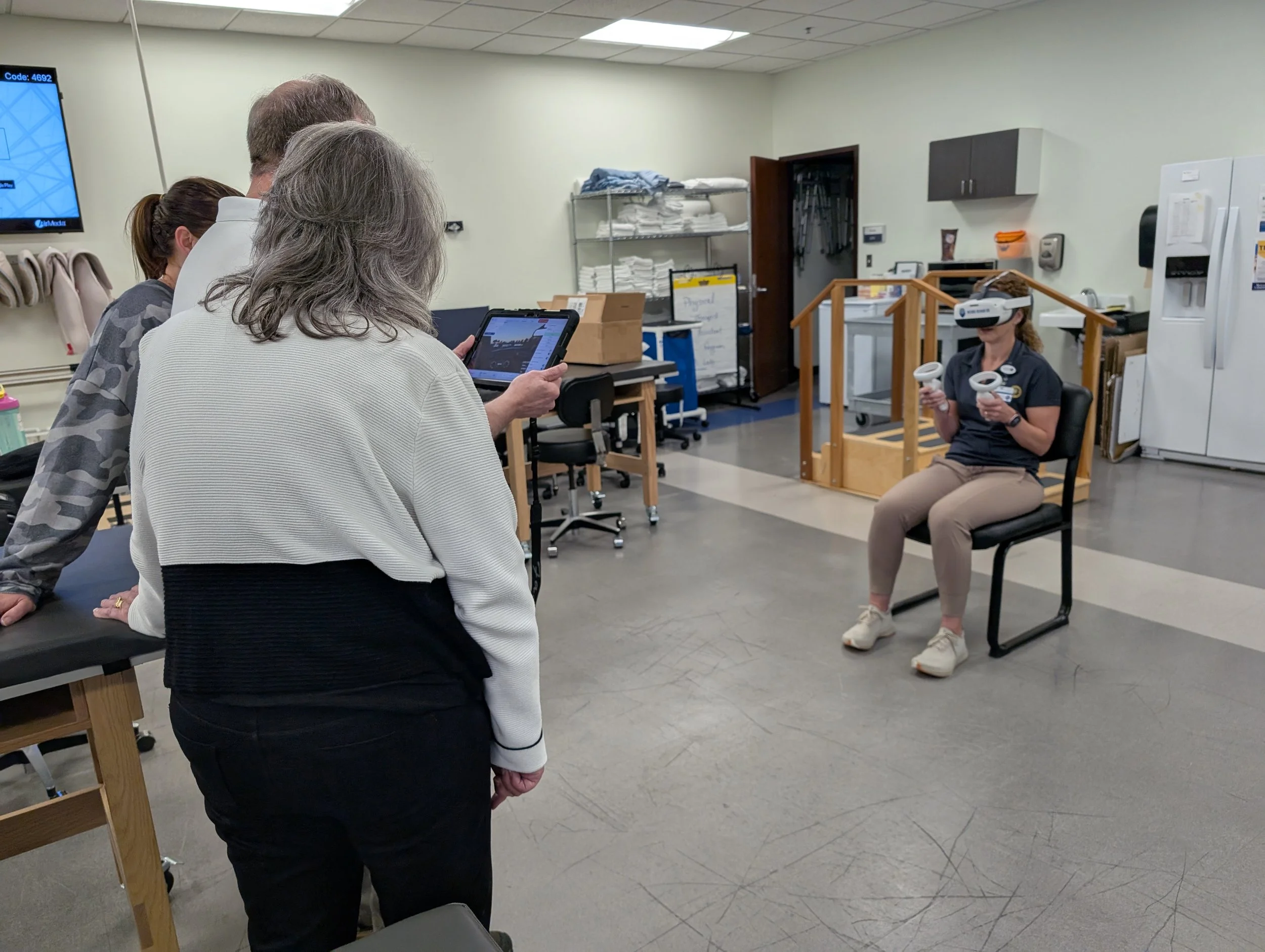
At Neuro Rehab VR, we believe that every step matters—and every step should be meaningful. Our Smart Therapy™ Complete Solution combines immersive, interactive lower-limb and gait exercises with powerful clinical insights.
Therapists can choose from a library of VR gait environments—uneven terrain, virtual hiking trails, street-crossing simulations, and more. Each session adapts in difficulty based on the patient’s input, while built-in AI tools capture metrics like step timing, stride length, and balance shifts.
What makes our platform different?
Gamified Motivation – Patients don’t just “walk”—they complete missions, solve puzzles, and unlock levels.
Therapist Tools – Clinicians can monitor live progress, analyze gait symmetry, and modify exercises instantly.
Effortless Gait Training Anywhere – With compatible our solution, patients can easily begin gait therapy. No complex setup required, just step into a virtual environment and start moving, while clinicians monitor progress and adjust in real time.
And the results speak for themselves: Patients report feeling more confident in their walking abilities, and therapists report higher session adherence and more accurate insights into progress.
From Clinic to Community: Rebuilding Real-Life Function
The ultimate goal of gait training isn’t better performance on a treadmill, it’s better mobility in the real world. VR prepares patients for the unpredictability of everyday life: uneven sidewalks, sudden obstacles, curbs, stairs, and shifting surfaces.
One of the most compelling advantages of immersive virtual reality (VR) in rehabilitation is its ability to promote real-world skill transfer. In a study titled “Transfer of motor skill between virtual reality viewed using a head-mounted display and conventional screen environments“, participants who trained in a VR environment using a head-mounted display demonstrated significantly better transfer of motor skills to real-life navigation tasks compared to those who trained using conventional 2D screens.
The immersive nature of VR—engaging spatial awareness, depth perception, and full-body movement—appears to activate motor learning pathways more effectively than traditional interfaces. This means that skills practiced in VR, such as balance control, gait adjustments, or obstacle avoidance, are more likely to translate into improved functional mobility in everyday environments. These findings support VR's role as a powerful tool for enhancing the relevance and effectiveness of rehabilitation exercises.(Juliano and Liew)
Addressing Fear of Falling: A Hidden Barrier
Many patients aren’t just recovering physically, they’re battling fear. Fear of falling is a major barrier to mobility, especially in older adults. Even after regaining strength, fear can limit participation in daily activities and increase the risk of future falls due to stiff, cautious movement.
VR addresses this barrier head-on. Patients can practice high-risk scenarios such as crossing a street, walking in a crowded area, stepping off a curb, without real consequences. Repetition breeds familiarity, which reduces anxiety. Over time, patients begin to trust their bodies again.
Making Therapy Inclusive: VR for All Levels of Mobility
Another advantage of VR? Accessibility. Whether someone is wheelchair-bound, using assistive devices, or just beginning to take steps again, VR can be tailored to their unique needs.
Research:
Virtual reality (VR) can offer profound psychological and emotional benefits—even for individuals who may never regain full mobility. In a systematic review titled “The Effectiveness of Virtual Reality Exercise on Individual’s Physiological, Psychological and Rehabilitative Outcomes: A Systematic Review”, the researchers found that lifelong wheelchair users who experienced walking in a virtual environment reported increased motivation, emotional engagement, and a stronger desire to participate in rehabilitation.
Although VR cannot replace physical walking for those with permanent mobility limitations, the simulated experience of movement created a powerful sense of embodiment and agency. This virtual sensation of walking helped users reconnect with physical goals, boost their confidence, and view therapy more positively.
These findings underscore the importance of not only physical outcomes in rehabilitation, but also the emotional and psychological impact that immersive technologies can provide. (Qian et al.)
The Future of Gait Training: Where We’re Headed
As VR continues to evolve, we’re seeing promising additions:
Wearable sensors that provide more granular gait data.
Haptic feedback systems that simulate ground texture or joint resistance.
AI-powered personalization to optimize progress.
AR overlays that blend virtual cues with real-world walking tasks.
Eventually, we may even see VR-powered group gait classes, where patients walk through virtual cities together, building community and accountability in the process.
The vision is clear: more personalized, more engaging, more effective therapy that meets patients where they are—physically, emotionally, and neurologically.
Final Thoughts: Step Forward With Us
Whether you’re a therapist helping patients take their first post-stroke steps, or a patient facing the daunting task of walking after injury or illness, one thing is certain—you deserve tools that support every part of your journey. Rehabilitation is never just physical. It’s emotional. It’s psychological. It’s personal. And every step forward, no matter how small, is a triumph.
Virtual reality doesn’t replace the skill, care, or human connection that therapists bring—it amplifies it. It adds dimension, engagement, and real-time feedback in a way that traditional tools often can’t. With VR, therapy becomes more than a routine. It becomes a story of progress—a series of moments where your body remembers what it’s capable of, and your mind starts to believe it again.
For clinicians, VR means you can track movement with more precision, adapt challenges to each patient’s needs, and spark joy in the process. For patients, it means you’re no longer stuck counting reps in a fluorescent-lit room. You're walking through forests, crossing bridges, climbing stairs in a city square. You’re moving through your fears, doubts, and limits—and redefining what recovery looks like.
Lower-limb and gait rehabilitation isn’t easy. But VR offers a way to make it more human, more hopeful, and more effective. So whether you're taking your first step, your thousandth, or helping someone else find their footing—let’s keep moving forward.
Because sometimes, the belief that progress is possible is the most powerful step of all.
-
Juliano, Julia M., and Sook-Lei Liew. “Transfer of Motor Skill between Virtual Reality Viewed Using a Head-Mounted Display and Conventional Screen Environments.” Journal of NeuroEngineering and Rehabilitation, vol. 17, no. 1, 10 Apr. 2020, https://doi.org/10.1186/s12984-020-00678-2. Accessed 1 Sept. 2021.
Laver, Kate E, et al. “Virtual Reality for Stroke Rehabilitation.” Cochrane Database of Systematic Reviews, vol. 11, no. 11, 20 Nov. 2017, www.cochrane.org/CD008349/STROKE_virtual-reality-stroke-rehabilitation, https://doi.org/10.1002/14651858.cd008349.pub4.
Ochandorena-Acha, Mirari, et al. “Effectiveness of Virtual Reality on Functional Mobility during Treadmill Training in Children with Cerebral Palsy: A Single-Blind, Two-Arm Parallel Group Randomised Clinical Trial (VirtWalkCP Project).” BMJ Open, vol. 12, no. 11, Nov. 2022, p. e061988, https://doi.org/10.1136/bmjopen-2022-061988.
Qian, Jiali, et al. “The Effectiveness of Virtual Reality Exercise on Individual’s Physiological, Psychological and Rehabilitative Outcomes: A Systematic Review.” International Journal of Environmental Research and Public Health, vol. 17, no. 11, 10 June 2020, p. 4133, https://doi.org/10.3390/ijerph17114133.
Raffegeau, Tiphanie E, et al. “A Perspective on Using Virtual Reality to Incorporate the Affective Context of Everyday Falls into Fall Prevention.” JMIR Aging, vol. 6, 11 Jan. 2023, p. e36325, https://doi.org/10.2196/36325.
Xiao, Xiang, et al. “Cerebral Reorganization in Subacute Stroke Survivors after Virtual Reality-Based Training: A Preliminary Study.” Behavioural Neurology, vol. 2017, 1 Jan. 2017, pp. 1–8, https://doi.org/10.1155/2017/6261479.