Reclaiming Life: VR Sparks Healing in the ICU
Written by: Brianna Hodge
If you've ever spent time in an ICU, or know someone who has, you understand that the road to recovery is long, uncertain, and often terrifying. For patients, being confined to a bed in a sterile, disorienting environment can be both physically limiting and emotionally exhausting. For clinicians, the challenge is immense: how do you safely mobilize someone in critical condition without jeopardizing their recovery?
Enter Virtual Reality (VR). It might seem counterintuitive at first, why would a critically ill patient need VR? But when used appropriately, VR can be a game-changing tool for early mobilization in ICU and acute care settings. It’s not just a tech gimmick, it’s a clinically validated approach that merges physical rehabilitation with emotional support, enhancing both patient outcomes and provider workflows.
Let’s walk through the science, real-world applications, and future potential of VR in one of the most delicate clinical spaces: the ICU.
Rowan-Cabarrus Community College
The Clinical Importance of Early Mobilization in ICU Settings
Prolonged immobility in the ICU is one of the most significant predictors of poor outcomes. ICU-acquired weakness (ICU-AW), functional decline, delirium, and extended ventilator dependency are just some of the risks associated with bedrest.
Research:
In the comprehensive review Mobilizing Progress: A Comprehensive Review of the Efficacy of Early Mobilization Therapy in the Intensive Care Unit, researchers reinforced the growing consensus that early mobilization offers critical benefits for ICU patients.
The study found that early initiation of movement-based interventions significantly improved both muscle strength and functional mobility, two key indicators of recovery. Importantly, it also demonstrated that patients who engaged in early mobilization experienced shorter ICU stays and fewer days on mechanical ventilation.
These findings underscore the importance of moving beyond passive care models and incorporating proactive, movement-oriented therapies into ICU protocols to support faster, more complete patient recovery (Singam).
The challenge? Mobilizing patients in the ICU isn’t simple. Intubation, sedation, monitoring lines, and unstable vitals create barriers. Therapists often have to balance the benefits of movement with the risks of overstimulation or physiological instability. This is where VR offers something special: the opportunity to engage patients without overexerting them, using environments that encourage participation while monitoring physiological thresholds.
How VR Works in ICU and Acute Care
Virtual Reality in this setting is not about full-body gaming or high-intensity tasks. Instead, it's carefully curated, medically appropriate content designed to stimulate the mind and gently encourage movement. Especially upper extremity movement, head turns, and visual tracking.
Here’s how it typically works:
Immersive distraction therapy: Patients are transported to calming environments like forests, beaches, or quiet villages. These experiences reduce anxiety and stress, allowing for gradual movement.
Active engagement: VR content can guide patients to reach out, turn their heads, or visually follow moving objects. All activities that encourage motor planning and neuromuscular reactivation.
Biofeedback and monitoring: Some systems can monitor heart rate, respiration, or oxygen levels in real-time to ensure patient safety.
Adaptive experiences: For patients unable to move, even passive VR (e.g., guided nature walks) can lower cortisol levels and reduce sedation needs, making mobilization easier later on.
Immersive Relief: Integrating VR into ICU Pain and Anxiety Management
The study Opportunities for Managing Pain and Anxiety in the Intensive Care Unit Using Virtual Reality: Perspectives from Bedside Care Providers highlights the promising role of VR as a non-pharmacological tool in ICU pain management. According to bedside providers, integrating VR into the treatment plans of critically ill patients offered a valuable way to reduce reliance on opioids while enhancing patient comfort.
Clinicians observed that VR created immersive distractions that helped patients manage acute pain episodes more calmly and with greater emotional regulation. Many also noted that VR could serve as a complementary therapy, especially during procedures or physical therapy sessions, by shifting patients’ focus away from discomfort and toward relaxing or engaging virtual environments.
These findings suggest that VR is not only feasible in the ICU but may fill an important gap in multimodal pain management strategies (Garito et al.).
The Psychological Side: Combating ICU Delirium and Emotional Trauma
If you’ve ever spoken to someone who’s been through an ICU stay, they might describe hallucinations, fear, confusion, or even PTSD-like symptoms. ICU delirium is real and frightening.
Research:
The study Feasibility of a Virtual Reality Intervention in the Intensive Care Unit explores the use of VR as a novel approach to combat ICU delirium, a condition that affects up to 80% of mechanically ventilated patients and is associated with long-term cognitive impairment. The researchers demonstrated that VR was not only safe and well-tolerated by critically ill patients but also showed potential in promoting cognitive engagement and orientation.
Patients who used VR reported feeling more connected to their environment and less anxious or disoriented, a critical step in reducing the severity and duration of delirium. The intervention provided immersive, calming experiences that helped reorient patients and served as a therapeutic alternative to traditional sedation strategies.
This study highlights VR’s emerging role in supporting neurocognitive health during some of the most vulnerable phases of critical care (Jawed et al.).
By providing a sense of escape and grounding at the same time, VR may help reduce the incidence and severity of ICU delirium, one of the costliest and most dangerous complications of prolonged ICU care.
Practical Implementation: What Does It Look Like?
One might imagine that VR requires lots of space, time, and setup, but this is not true. In most clinical settings, VR can be implemented using:
A single headset with hygienic covers
A tablet or remote to launch and control sessions
Battery-powered operation (no cords or complex setup)
A content library that meets rehab and relaxation goals
A typical session in the ICU might last 5–15 minutes, especially in early stages. It could involve something as simple as looking around a 360° nature environment, breathing exercises, or music therapy.
Importantly, clinicians remain in control. They monitor vitals, adjust session time, and can pause or switch content as needed. As more hospitals adopt VR, we’re seeing streamlined protocols for its use in step-down units and acute care wards.
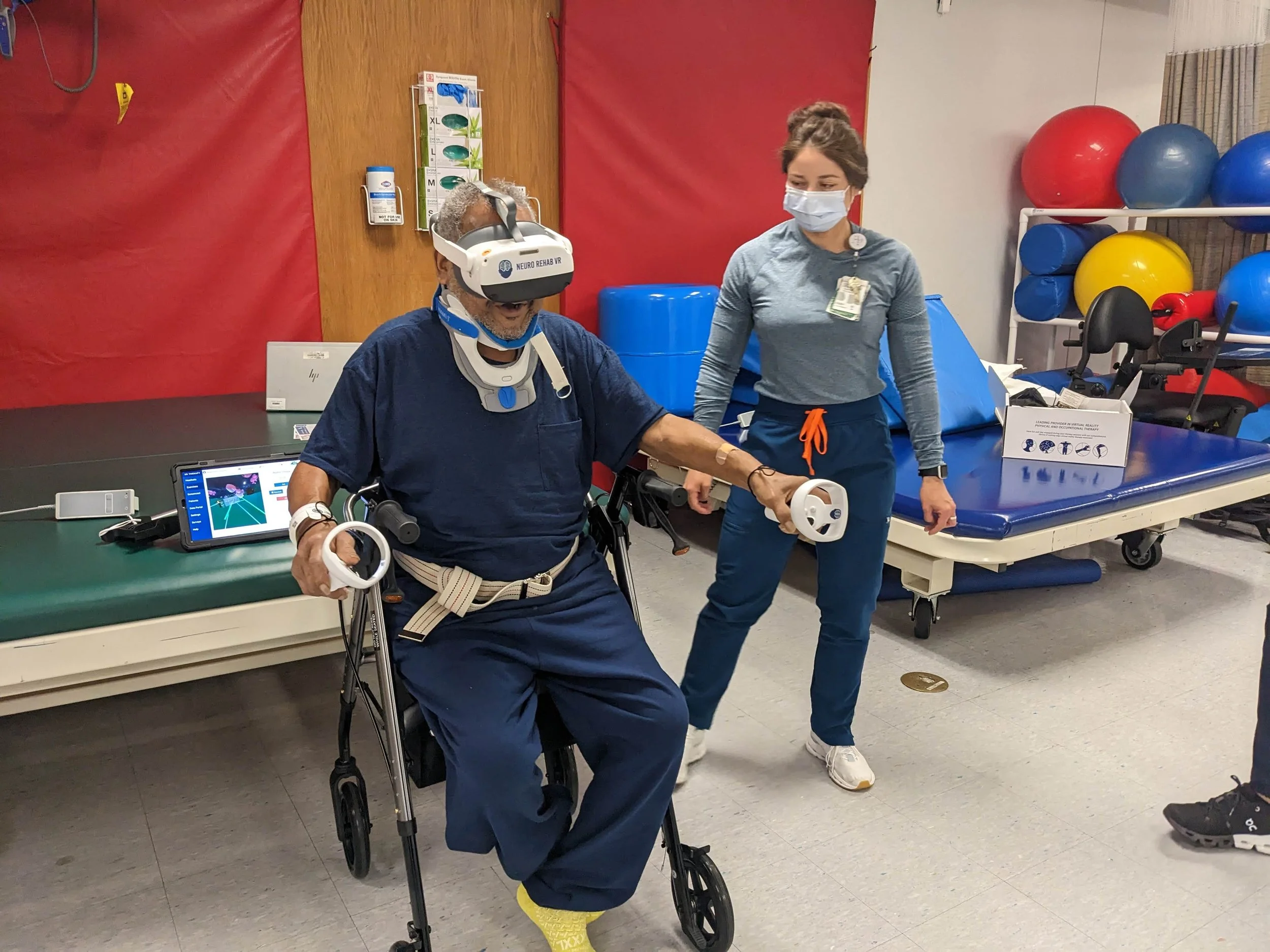
Neuro Rehab VR: Bringing Smart Therapy to Critical Care
One of the leaders in this space is Neuro Rehab VR, which has developed a Smart Therapy Complete Solution for acute, ICU, and neurorehabilitation settings. What sets them apart isn’t just their immersive content—but their focus on clinician needs and workflow optimization.
With Neuro Rehab VR’s platform:
Therapists can select from activities focused on mobility, cognitive stimulation, relaxation, or strength-building.
Sessions are adaptable, allowing patients to participate even when bed-bound or on minimal movement orders.
Data is captured and used to generate documentation for progress tracking and note generation, streamlining workflows for overworked ICU therapists.
Their activities include environments like calm villages, interactive scenarios for early upper limb mobilization, and meditation for respiratory support.
In a real-world deployment at Encompass Health, therapists used Neuro Rehab VR with stroke and ICU step-down patients who were hesitant to move. The patients reported increased motivation and participated in more minutes of therapy, and therapists noted a decrease in behavioral refusals.
Research Backing: What the Science Says
Let’s look at some of the published research on VR in early mobilization:
Research 1:
The randomized pilot study Effectiveness of Virtual Reality Assisted Active Limb Movement Exercises for Patients in the Respiratory Intensive Care Unit provides compelling evidence that VR-assisted rehabilitation can significantly enhance physical function in critically ill patients.
Conducted in a respiratory ICU, the study compared traditional therapy to VR-assisted limb movement exercises and found that patients in the VR group demonstrated improved upper limb muscle strength and functional outcomes. The immersive nature of VR helped increase patient engagement and motivation, making repetitive exercises more tolerable and even enjoyable. Importantly, the intervention was safe and well-tolerated, with no adverse effects reported.
This research reinforces the value of VR as a practical and effective adjunct to early physical therapy in the ICU, supporting faster recovery and greater patient participation during a vulnerable stage of care (Wang et al.).
Research 2:
Postintensive Care Syndrome highlights the psychological benefits of VR for patients recovering from critical illness. Postintensive care syndrome (PICS), which includes symptoms like anxiety, depression, PTSD, and cognitive dysfunction, is a common yet often under-addressed consequence of ICU stays.
This study found that VR interventions led to significant psychological improvements, including reduced stress levels, better emotional regulation, and enhanced overall mental well-being. Patients who engaged with immersive VR content felt more in control of their recovery and more connected to their surroundings. By recreating familiar environments or offering calming experiences, VR provided therapeutic reorientation that traditional interventions often fail to achieve.
These findings support VR’s potential as a powerful tool in the post-ICU recovery process, helping patients rebuild not just their bodies but their sense of self (Vlake et al.).
This isn't experimental anymore. It's real, it’s happening now, and it’s proving itself every day in hospitals and rehab centers around the world.
Challenges to Address
Of course, it’s not all smooth sailing. There are some barriers to address:
Infection control: VR headsets must be sanitized rigorously between uses.
Training: Staff need to be trained not just in the tech but in how to integrate it safely into critical care workflows.
Patient appropriateness: Not all ICU patients are candidates for VR. Clear clinical criteria are essential.
Technology acceptance: Some clinicians and administrators still view VR as novel or unnecessary, and that cultural shift takes time and evidence.
However, none of these challenges are insurmountable. As research mounts and more frontline teams adopt the technology, best practices are emerging rapidly.
What This Means for You—Whether You’re a Clinician or a Family Member
If you’re a clinician, think of VR not as a replacement for your work, but as a powerful new tool in your therapy kit. Whether you're an OT, PT, nurse, or physician, VR can help you reach patients who otherwise disengage or plateau. It’s particularly helpful when traditional mobility is limited but engagement is still crucial.
If you’re a family member or caregiver, this is a sign of hope. Early mobilization through VR can help your loved one stay oriented, reduce their emotional distress, and potentially shorten their stay or reduce long-term complications.
We’re not talking about the distant future here, we’re talking about today’s best hospitals making innovative choices that protect and empower the most vulnerable patients.
Conclusion: The ICU Doesn’t Have to Be Isolating
We often imagine the ICU as a place of stillness and silence, but it doesn't have to be. With VR, we’re adding movement, presence, calm, and even joy into those quiet, high-stakes moments. It’s helping patients find their way back to their bodies and their lives by providing help in a faster, more safer, and less fearful way.
The next time you see a VR headset in a hospital, don’t think “gimmick.” Think “gateway.” Because sometimes, the path out of the ICU starts with a single deep breath… while watching the waves crash in VR.
-
Garito, Isabella P, et al. “Opportunities for Managing Pain and Anxiety in the Intensive Care Unit Using Virtual Reality: Perspectives from Bedside Care Providers.” Journal of Medical Extended Reality, vol. 1, no. 1, 1 Mar. 2024, pp. 53–64, https://doi.org/10.1089/jmxr.2023.0007.
Jawed, Yameena T., et al. “Feasibility of a Virtual Reality Intervention in the Intensive Care Unit.” Heart & Lung, vol. 50, no. 6, Nov. 2021, pp. 748–753, https://doi.org/10.1016/j.hrtlng.2021.05.007.
Singam, Amol . “Mobilizing Progress: A Comprehensive Review of the Efficacy of Early Mobilization Therapy in the Intensive Care Unit.” Curēus, vol. 16, no. 4, 4 Apr. 2024, https://doi.org/10.7759/cureus.57595.
Vlake, Johan H., et al. “Virtual Reality to Improve Sequelae of the Postintensive Care Syndrome: A Multicenter, Randomized Controlled Feasibility Study.” Critical Care Explorations, vol. 3, no. 9, Sept. 2021, p. e0538, https://doi.org/10.1097/cce.0000000000000538. Accessed 17 Mar. 2022.
Wang, Jiani, et al. “Effectiveness of Virtual Reality Assisted Active Limb Movement Exercises for Patients in the Respiratory Intensive Care Unit: A Randomized Pilot Study.” Journal of Rehabilitation Medicine, vol. 57, 3 June 2025, p. jrm28399, pmc.ncbi.nlm.nih.gov/articles/PMC12160588/, https://doi.org/10.2340/jrm.v57.28399.