Rewiring Recovery: VR’s Power to Build New Habits
Written by: Brianna Hodge
If you've ever tried to start a workout regimen, eat healthier, or improve your sleep, you already know how hard forming a new habit can be. Now imagine that you're recovering from a stroke, traumatic brain injury, or a chronic neurological condition. In those circumstances, habit formation isn't just helpful, it’s essential.
Therapeutic routines drive long-term recovery. But sticking to those routines? That’s where many patients falter. Repetition becomes monotonous. Progress can feel invisible. And even the most well-meaning therapists can't follow you home to keep you on track.
This is where virtual reality (VR) changes the game. Far beyond flashy tech, VR has proven its ability to create immersive, personalized, and neurologically engaging environments that support one of the most critical elements of rehab success: habit formation.
Let’s explore the psychology, science, and real-world impact of VR on habit-building in rehabilitation.
Rowan-Cabarrus Community College
The Psychology of Habit Formation in Rehab
At its core, a habit is a behavior loop: cue, action, and reward. In rehabilitation, this might look like:
Cue: Entering the clinic or hearing a reminder alert
Action: Completing a therapy exercise
Reward: A sense of accomplishment or improved movement
But this loop is fragile, especially when motivation fades, tasks feel tedious, or patients don’t see immediate results.
Research:
A key component of habit formation lies in the brain’s reward system,specifically, how it evaluates and reinforces behavior. According to The Brain’s Reward System in Health and Disease, the dopaminergic pathways, particularly those involving the mesolimbic system, play a critical role in motivating actions by signaling reward prediction and reinforcing outcomes.
When a behavior consistently leads to a pleasurable or meaningful outcome, the brain is more likely to encode it as a habit. In rehabilitation, this mechanism becomes vital. If therapeutic exercises feel rewarding—whether through improved function, reduced pain, or even engaging VR environments that offer visual and auditory feedback, the brain strengthens the association between the routine and its positive results.
This not only increases motivation in the short term but also encourages long-term repetition, which is essential for neural recovery and functional improvement after injury or illness. (Lewis et al.)
That’s why VR offers such an important bridge. It doesn't just instruct movement, it transforms it into a sensory experience with built-in feedback, challenge, and progress indicators.
VR: A Neurological Shortcut to Habit Loops
Why is VR so effective at encouraging new habits? Because it leverages key components of brain plasticity, motivation, and engagement:
Multisensory Stimulation: VR involves vision, proprioception, balance, and often auditory input, activating multiple brain regions simultaneously.
Reward Systems: Gamified elements, visual feedback, and performance scores stimulate the brain’s reward center, reinforcing repetition.
Contextual Learning: Patients can perform exercises in familiar or meaningful environments, from virtual grocery stores to kitchen simulations—activating memory and contextual association.
Autonomy and Control: Patients become active participants in their therapy, choosing scenarios and navigating space, which increases intrinsic motivation.
The Role of Immersion in Behavioral Repetition
When a task feels rewarding, we're more likely to repeat it. VR leverages this by wrapping therapeutic movements in engaging, purpose-driven activities.
For example:
Instead of lifting your arm 15 times, you’re reaching for apples in an orchard.
Instead of walking down a hallway, you’re exploring a forest trail.
These aren’t distractions—they’re carefully constructed environments that prompt physical effort while providing cognitive stimulation, visual reward, and emotional context.
Research:
In the article Use of Virtual Reality in Physical Therapy as an Intervention and Diagnostic Tool, researchers highlight a significant advantage of VR in rehabilitation: improved patient adherence and reduced dropout rates.
Patients engaged in VR-based therapy were more likely to complete their sessions consistently compared to those undergoing traditional therapy approaches. This difference is largely attributed to the motivational power of immersive feedback loops. Unlike conventional exercises that can feel repetitive and uninspiring, VR environments provide immediate, engaging, and often gamified responses to movement—offering patients a sense of progress and reward in real time. These interactive elements activate the brain’s reward system, reinforcing behavior and encouraging patients to stick with their therapy routines.
In the context of long-term recovery, especially for individuals with neurological or orthopedic conditions, this increased adherence can translate into better outcomes and more sustainable functional gains.(Bateni et al.)
It’s not just that VR is more fun, it’s that it taps into the reward cycle that builds the neural pathways necessary for long-term behavioral change.
Habit Reinforcement Through Real-Time Feedback
One of the most powerful components of VR therapy is real-time feedback. Patients get instant information on their movement quality, accuracy, speed, and symmetry. This immediate feedback loop accelerates learning and supports motor memory retention.
Contrast this with traditional therapy, where feedback is often delayed until after the movement is complete, or even after the session ends. Without timely reinforcement, the brain struggles to associate action with reward.
In VR environments, the moment you lift your leg high enough, a visual cue lights up. When your balance improves, you unlock a new level or score. This feedback is essential for helping patients form internal models of “what right feels like.”
Research:
The narrative review Exploring the Efficacy of Virtual Reality-Based Rehabilitation in Stroke emphasizes the substantial benefits of VR-based biofeedback systems in enhancing rehabilitation outcomes, particularly for patients with cognitive impairments. These systems deliver real-time feedback on movement accuracy, speed, and effort, which is crucial for reinforcing correct motor patterns and maintaining patient engagement.
For stroke survivors, many of whom struggle with deficits in attention, memory, or executive function, this immediate and continuous feedback acts as both a guide and motivator, helping to sustain focus and encourage repetition. By making each movement meaningful and measurable, VR creates a more structured and rewarding therapy experience that supports motor learning even in the presence of cognitive challenges.
This ability to personalize and adapt therapy in the moment is one of VR’s greatest strengths in driving both neuroplastic change and long-term functional gains.(Aderinto et al.)
Repetition Without the Monotony
Let’s face it, rehab is hard. It takes grit, time, and often many repetitions before functional changes appear. This is especially true for patients recovering from neurological injuries, where thousands of practice reps might be needed to relearn basic motor functions.
But repetition without meaning quickly becomes a chore. VR reshapes repetition into challenge and novelty. The same core movement might appear across dozens of different virtual environments, each one providing new context, visuals, and narrative.
This is especially useful for maintaining motivation over long rehab timelines. A task that would otherwise feel tedious, like lifting the arm or standing from a chair, can become part of an archery challenge, a cooking game, or a balance test on a virtual mountain ridge.
Research:
In the article The Untapped Potential of Virtual Reality in Rehabilitation of Balance and Gait in Neurological Disorders, the authors emphasize how VR can transform repetitive rehabilitation tasks into dynamic, engaging experiences, effectively addressing one of the biggest challenges in therapy: monotony.
Traditional balance and gait training often rely on static routines that can lead to disengagement over time. However, VR introduces variation, interactivity, and purpose into these exercises, allowing patients to perform necessary movements within immersive, goal-oriented environments. Whether navigating a bustling virtual street or balancing on a simulated hiking trail, patients repeat core motions without the mental fatigue associated with doing the same task over and over again.
This infusion of novelty maintains motivation, improves adherence, and helps reinforce neuromuscular patterns in ways that feel less like treatment and more like exploration. By offering repetition without monotony, VR sustains the intensity and frequency required for meaningful neurological recovery. (Keshner and Lamontagne)
Stroke Recovery and Habit Formation
In the study Virtual Reality for the Rehabilitation of the Upper Limb Motor Function After Stroke, researchers evaluated how virtual reality could enhance traditional therapy outcomes by dividing post-stroke patients into two groups. One group underwent conventional upper limb conventional (ULC) therapy, while the other group received the same therapy supplemented with VR-based training.
The findings revealed that the group incorporating VR achieved significantly better outcomes in upper limb motor function. This was largely attributed to the immersive and interactive nature of VR, which encouraged patients to engage more fully with their exercises and complete more repetitions with higher motivation. The virtual tasks were specifically designed to mimic real-world arm movements, providing both challenge and reward through real-time visual and auditory feedback.
By combining VR with ULC therapy, the intervention not only improved motor performance but also made the rehabilitation experience more stimulating and sustainable for patients recovering from stroke. (Turolla et al.)
From Clinic to Couch: Home-Based VR and Daily Consistency
One of the most exciting areas of VR in rehabilitation is home-based systems. These portable VR headsets allow patients to continue therapy outside the clinic, giving them ownership over their schedule and pace.
This consistent access is key to habit formation. When patients can perform therapy in their living room without waiting for a weekly appointment, they’re more likely to build a daily rhythm.
Research:
The study Improving Adherence to Physical Therapy in the Development of Serious Games: Conceptual Framework Design Study sheds light on a critical advantage of home-based VR programs: their ability to foster significantly higher adherence rates compared to traditional home therapy formats such as paper-based worksheets or mobile apps.
Researchers found that patients were more likely to stick with their prescribed exercises when those exercises were delivered through immersive, interactive VR experiences. Participants specifically cited “immersion,” “fun,” and “clear goals” as the primary motivators behind their sustained engagement. Unlike conventional approaches that often lack feedback or stimulation, VR therapy provides a compelling environment that keeps patients focused, motivated, and aware of their progress.
This sense of purpose and enjoyment helps build a consistent habit of participation, one of the most vital factors in achieving long-term rehabilitation outcomes, especially in a home setting where external accountability is limited.(Ambros-Antemate et al.)
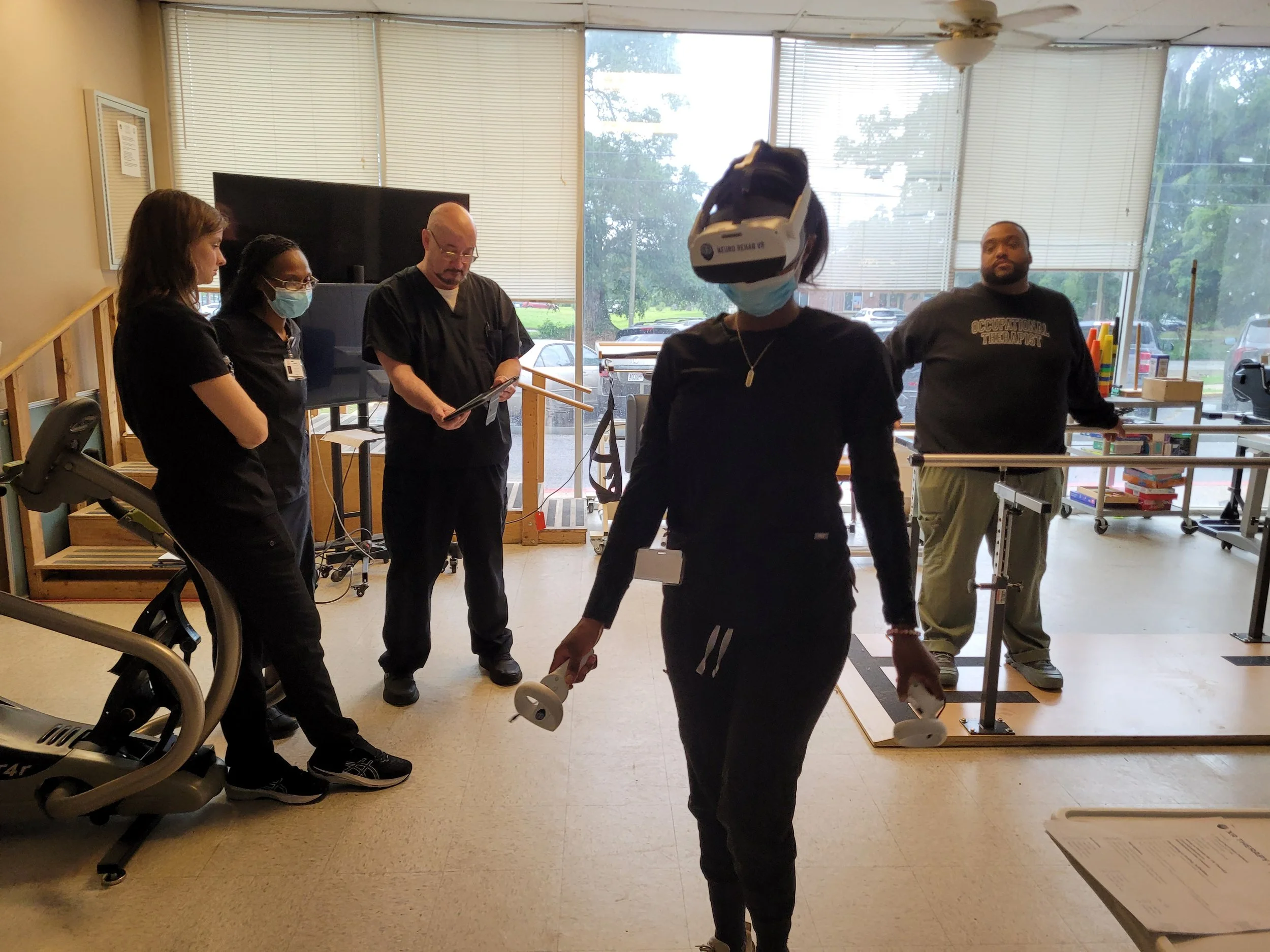
Neuro Rehab VR: Supporting Habit Formation with Smart Therapy™
At Neuro Rehab VR, habit-building is built into the system design. Every game, movement, and feedback loop is crafted not just to improve motor function, but to encourage consistent, long-term participation.
The Smart Therapy™ Complete Solution provides:
Gamified Therapy: Activities that are rewarding, visually engaging, and progressively challenging.
Adaptive Feedback: Real-time feedback helps patients track progress and stay motivated.
Clinician Support Tools: Therapists can track trends, customize programs, and ensure exercises remain fresh and meaningful.
In one internal review, 92% of patients using Neuro Rehab VR reported higher motivation to complete their rehab routines when compared to prior approaches. More importantly, therapists noted a reduction in skipped sessions, less drop-off after discharge, and more frequent reports of “therapy becoming a part of daily life.”
Habit Formation in Cognitive and Emotional Rehab
It’s not just physical routines that benefit from habit-building in VR. Cognitive training, mindfulness, and emotional regulation also see significant improvements when embedded into immersive routines.
For example, individuals with traumatic brain injury or mild cognitive impairment often need to practice memory, attention, and executive function skills consistently. But traditional worksheets and tabletop tasks rarely engage them long enough to build strong habits.
VR offers alternate environments for memory recall games, planning tasks, and emotional regulation activities. When these are engaging and contextually relevant—like remembering a grocery list in a virtual supermarket, the likelihood of forming a habit increases.
Research:
The scoping review Exploring Virtual Reality-Based Reminiscence Therapy on Cognitive and Emotional Well-Being in People with Cognitive Impairments concluded that VR-based cognitive therapy offers stronger and more sustained improvements in key cognitive domains, particularly working memory and attention, when compared to conventional therapeutic methods.
One of the primary reasons for these enhanced outcomes was the higher level of patient engagement and repeated use associated with VR interventions. The immersive nature of VR creates a stimulating, multisensory environment that captures attention and encourages patients to return to the therapy regularly, fostering consistency and cognitive reinforcement over time.
Unlike standard exercises that can become repetitive and disengaging, VR scenarios, especially those involving reminiscence or meaningful personal experiences, provide emotional resonance and mental stimulation. Which are crucial for supporting cognitive rehabilitation in individuals with memory or attention deficits. (Pardini et al.)
Therapist Perspective: A Partner in the Habit Loop
Therapists aren’t replaced by VR, they’re empowered by it.
When clinicians can see real-time performance data, adjust challenges, and automate parts of the feedback loop, they can shift their focus to what really matters: helping patients build sustainable behavior change.
For many therapists, this means being able to:
Monitor at-home participation without guesswork
Deliver motivating messages based on patient trends
Focus on emotional support and personal goal alignment
Reduce the monotony of assigning “more reps” by turning tasks into engaging routines
In essence, therapists become behavior coaches, partnering with technology to reinforce habits both inside and outside the clinic.
The Future: AI and Personalization in Habit Loops
As artificial intelligence and machine learning continue to integrate with VR platforms, the future of habit formation will become even more personalized.
Imagine a VR system that:
Adjusts difficulty based on your fatigue level
Reminds you to stretch at a specific time of day
Changes the environment when it detects boredom
Encourages reflection when progress plateaus
This isn’t science fiction, it’s the logical next step in neuroadaptive rehabilitation. And as systems like Neuro Rehab VR continue to evolve, the goal isn’t just more therapy, it’s better habits that patients carry into the rest of their lives.
Conclusion: Consistency Is the New Goal
Rehabilitation is not just about recovery, it’s about transformation. And transformation only happens through consistent action.
Virtual reality therapy has emerged as one of the most powerful tools for building those consistent actions into habits. By creating environments that are immersive, meaningful, and rewarding, VR makes it easier for patients to start, stick with, and succeed in long-term rehab routines.
You’re not just repeating a movement, you’re stepping into a new way of living. And with each session, your brain is learning to expect, enjoy, and crave the activity that helps it heal.
So if you’re a patient, a caregiver, or a therapist, remember this: habits are what turn hope into progress. And VR is here to help you build them.
-
Aderinto, Nicholas, et al. “Exploring the Efficacy of Virtual Reality-Based Rehabilitation in Stroke: A Narrative Review of Current Evidence.” Annals of Medicine, vol. 55, no. 2, 27 Nov. 2023, https://doi.org/10.1080/07853890.2023.2285907.
Ambros-Antemate, Jorge Fernando, et al. “Improving Adherence to Physical Therapy in the Development of Serious Games: Conceptual Framework Design Study.” JMIR Formative Research, vol. 7, 10 Nov. 2023, p. e39838, www.ncbi.nlm.nih.gov/pmc/articles/PMC10674146/, https://doi.org/10.2196/39838.
Bateni, Hamid , et al. “Use of Virtual Reality in Physical Therapy as an Intervention and Diagnostic Tool.” Rehabilitation Research and Practice, vol. 2024, 25 Jan. 2024, pp. 1–9, pmc.ncbi.nlm.nih.gov/articles/PMC10834096/, https://doi.org/10.1155/2024/1122286.
Keshner, Emily A., and Anouk Lamontagne. “The Untapped Potential of Virtual Reality in Rehabilitation of Balance and Gait in Neurological Disorders.” Frontiers in Virtual Reality, vol. 2, 11 Mar. 2021, https://doi.org/10.3389/frvir.2021.641650.
Lewis, Robert G., et al. “The Brain’s Reward System in Health and Disease.” Advances in Experimental Medicine and Biology, vol. 1344, no. 1344, 2021, pp. 57–69, pmc.ncbi.nlm.nih.gov/articles/PMC8992377/, https://doi.org/10.1007/978-3-030-81147-1_4.
Pardini, Susanna, et al. “Exploring Virtual Reality-Based Reminiscence Therapy on Cognitive and Emotional Well-Being in People with Cognitive Impairments: A Scoping Review.” Brain Sciences, vol. 15, no. 5, 13 May 2025, p. 500, www.mdpi.com/2076-3425/15/5/500, https://doi.org/10.3390/brainsci15050500.
Turolla, Andrea, et al. “Virtual Reality for the Rehabilitation of the Upper Limb Motor Function after Stroke: A Prospective Controlled Trial.” Journal of Neuroengineering and Rehabilitation, vol. 10, no. 85, 2013, p. 85, www.ncbi.nlm.nih.gov/pubmed/23914733, https://doi.org/10.1186/1743-0003-10-85.