Holiday Stress And Emotional Resilience In Physical Therapy
Written by: Brianna Hodge
December is a different month in the physical therapy clinic.
You feel it the moment a patient walks in slower than usual. You hear it when someone says, “I almost canceled today, it’s just been a lot.” You see it when attention drifts during exercises that felt automatic just weeks ago. And if you’re honest, you feel it in yourself too.
The holidays bring more than decorations and time off requests. They bring increased cognitive load, emotional stress, disrupted routines, and physical fatigue. All of which directly affect movement quality, learning, and engagement in physical therapy.
This blog is written for you, the physical therapist who’s trying to keep patients moving forward in December without pushing them past their limits. We’re going to talk about how the holiday season impacts cognitive load, emotional resilience, and patient engagement in PT. And how you can adapt your clinical approach to support patients while still protecting your own energy.
Understanding Cognitive Load in Physical Therapy During the Holidays
In physical therapy, cognitive load matters more than we sometimes acknowledge.
Every exercise requires attention, sequencing, body awareness, motor planning, and feedback processing. Whether you’re retraining gait, working on balance, teaching post-op precautions, or progressing a strengthening program, patients must mentally engage with their bodies for learning to occur.
In December, that mental bandwidth is already stretched thin.
Patients are juggling:
Changes in daily routines
Increased social and family obligations
Financial stress
Travel and sleep disruption
Seasonal mood changes
Pain flare-ups due to cold weather or stress
When cognitive load outside the clinic increases, capacity inside the clinic decreases. This directly impacts a patient’s ability to concentrate on form, retain cues, tolerate frustration, and stay engaged with their physical therapy plan of care.
Holiday Stress Through a Physical Therapy Lens
The article “Stress During the Holidays: A Physical Therapist’s Perspective” speaks directly to what PTs see every December: stress doesn’t just affect mood, it affects movement, pain, and recovery.
The author describes how increased stress leads to higher muscle tension, exacerbation of chronic pain, and decreased tolerance for physical effort. From a PT standpoint, this means patients may demonstrate:
Increased guarding
Reduced range of motion
Higher pain reports without structural change
Faster fatigue during therapeutic exercise
Decreased consistency with home exercise programs
Stress activates the sympathetic nervous system, which interferes with motor control and recovery. For patients in neuro rehab, ortho rehab, or chronic pain management, this can slow progress even when objective impairments haven’t changed(Scott) .
As a physical therapist, recognizing this allows you to reframe December setbacks. The issue often isn’t the exercise itself, it’s the physiological and cognitive state the patient brings into the session.
Why Even “Happy” Holidays Increase Cognitive Load
The American Psychological Association’s report, “Even a Joyous Holiday Season Can Cause Stress for Most Americans,” provides critical context for physical therapists.
The APA found that the majority of Americans experience elevated stress during the holidays, even when they view the season positively. Planning, social interaction, financial decision-making, and emotional expectations all require mental effort.
For physical therapy patients, this matters because stress affects:
Attention and working memory
Sleep quality (which impacts tissue healing and motor learning)
Emotional regulation and pain perception
Motivation to engage in physically demanding tasks
In PT, we rely on repetition, consistency, and active participation. When stress is high, patients may appear “less motivated,” but in reality, they are operating at a cognitive deficit caused by overload, not lack of effort (American Psychological Association).
Patient Engagement in Physical Therapy: What the Research Shows
The systematic review “Identifying the factors affecting ‘patient engagement’ in exercise rehabilitation” provides a strong evidence-based foundation for understanding what happens in December.
The review identifies several key factors that influence engagement in physical therapy:
Emotional state and stress levels
Perceived relevance of exercises
Self-efficacy and confidence
Quality of the therapist–patient relationship
Environmental and contextual barriers
Importantly, the research emphasizes that engagement declines when patients feel overwhelmed or emotionally unsupported, even when exercises are clinically appropriate.
In December, patients are more likely to feel:
Mentally fatigued
Emotionally vulnerable
Less confident in their progress
Guilty for prioritizing therapy over family obligations
For PTs, this means engagement strategies that worked in October may fall flat in December unless they are adapted to the patient’s emotional and cognitive state (Teo et al.) .
Winter-Specific Barriers to Physical Therapy Engagement
The article “How To Keep Your Patients Engaged During the Winter Months” highlights practical challenges that physical therapists face as the season changes.
Winter brings:
Reduced daylight, which affects mood and energy
Cold temperatures that increase joint stiffness and pain
Higher illness rates leading to missed sessions
Increased fear of falling, especially in older adults
These factors can decrease willingness to move and reduce consistency with therapy attendance and home exercise programs. From a PT perspective, winter disengagement often shows up as shorter tolerance for sessions, hesitation with progression, or reduced carryover between visits (NARA) .
The article emphasizes the importance of variety, motivation, and adaptability in maintaining engagement, principles that become even more critical during the holiday season.
Supporting Emotional Resilience Without Compromising PT Outcomes
Supporting emotional resilience in physical therapy does not mean lowering clinical standards. It means adjusting how we deliver care so patients can continue progressing despite increased stress.
Here are PT-specific strategies that matter most in December:
1. Simplify Motor Demands
Reduce dual-tasking when appropriate. Focus on quality over quantity. Fewer exercises done well often outperform overloaded sessions.
2. Anchor Exercises to Functional Holiday Goals
Connect therapy to what patients care about right now, standing longer during gatherings, navigating crowded spaces, or managing fatigue while traveling.
3. Normalize Variability
Explain that fluctuations in pain, balance, or endurance are common during high-stress periods. This reduces fear and improves adherence.
4. Emphasize Wins
Small improvements matter. Reinforcing progress restores confidence, which directly supports motor learning and engagement.
5. Strengthen the Therapeutic Alliance
Research consistently shows that patients engage more when they feel emotionally supported by their physical therapist. December is when this relationship carries the most weight.
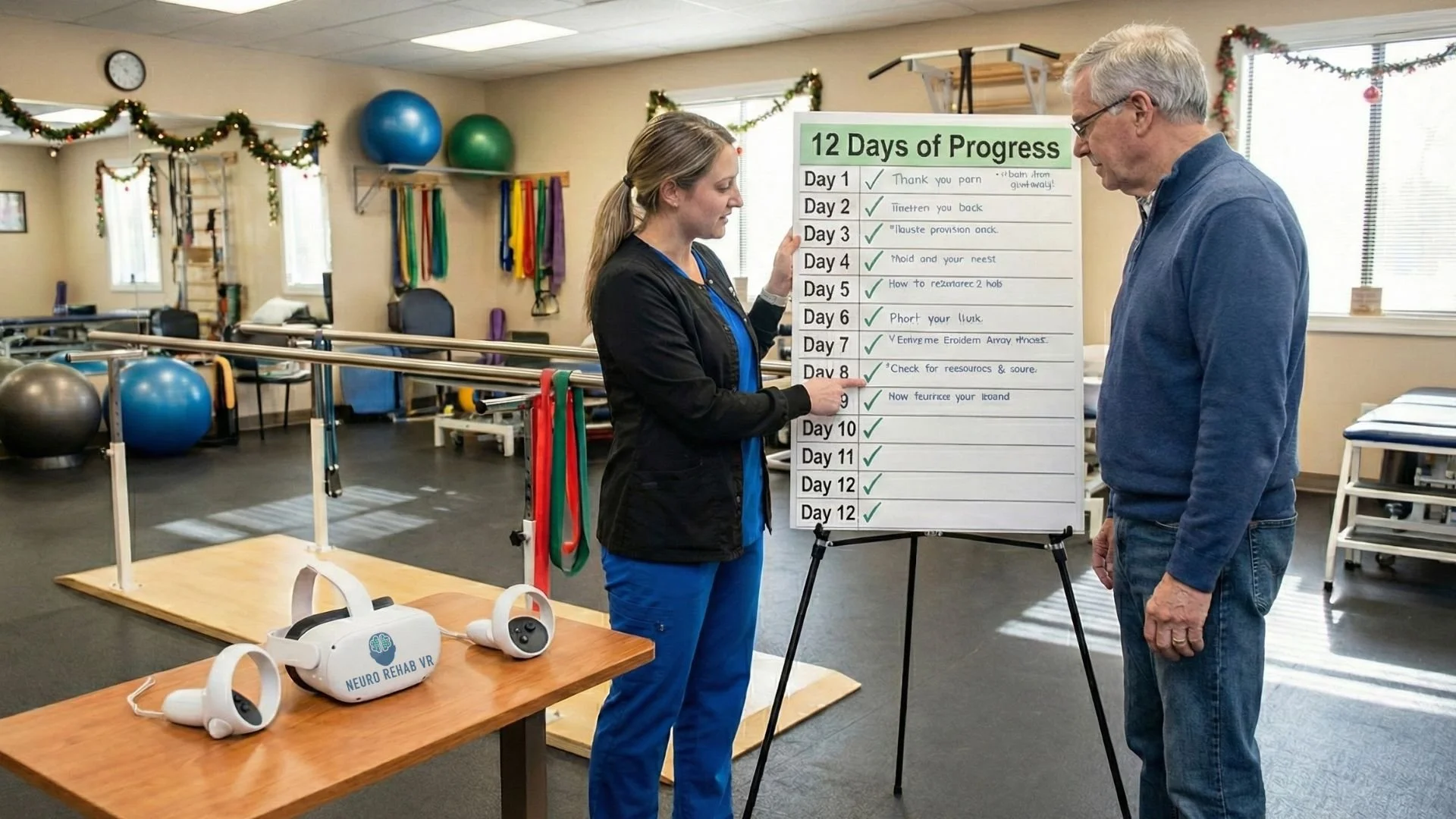
The Role of Neuro Rehab VR in December Physical Therapy Care
During periods of high cognitive and emotional load, tools that support engagement without increasing mental strain become especially valuable in physical therapy.
The Smart Therapy Complete Solution provides immersive, therapist-guided experiences that help patients stay present and motivated during PT sessions. For patients struggling with attention, fatigue, or emotional overwhelm, immersive environments can reduce external distractions and support focus on movement.
In physical therapy settings, Smart Therapy allows clinicians to:
Adjust task complexity in real time
Maintain repetition and intensity without monotony
Support patients with neurological, orthopedic, or balance impairments
Encourage active participation even when emotional resilience is low
Research has shown that immersive rehab tools can improve motivation, adherence, and patient satisfaction, all of which are critical during December, when engagement is most vulnerable.
Importantly, it supports rather than replaces skilled physical therapy. It enhances motor learning and emotional buy-in while allowing PTs to individualize care based on the patient’s cognitive and emotional capacity that day.
December Is Hard for PTs Too
Physical therapists aren’t immune to the season.
You’re managing higher emotional demands, tighter schedules, cancellations, productivity pressure, and your own personal obligations. Supporting patient resilience starts with recognizing your limits as well.
Understanding that December disengagement is often a stress response, not a lack of effort, can protect you from frustration and burnout. When expectations align with reality, care becomes more compassionate and sustainable.
Closing: December Isn’t a Regression, It’s a Clinical Reality
The holiday season doesn’t erase progress made in physical therapy. It tests how adaptable our care models are.
Patients who feel emotionally supported, cognitively respected, and functionally motivated can continue making gains, even in December. Not because the season is easy, but because physical therapy meets them where they are.
Your role this month isn’t to push harder. It’s to guide smarter, connect deeper, and support movement in the context of real life.
-
American Psychological Association. “Even a Joyous Holiday Season Can Cause Stress for Most Americans.” Apa.org, 2023, www.apa.org/news/press/releases/2023/11/holiday-season-stress.
NARA. “How to Keep Your Patients Engaged during the Winter Months.” Naranet.org, 2023, www.naranet.org/blog/post/how-to-keep-your-patients-engaged-during-the-winter-months-. Accessed 16 Dec. 2025.
Scott, Brianne. “Stress during the Holidays: A Physical Therapist’s Perspective.” Omegaprojectpt.com, 2025, www.omegaprojectpt.com/blog/stress-during-the-holidays-a-physical-therapists-perspective/.
Teo, Junsheng L., et al. “Identifying the Factors Affecting “Patient Engagement” in Exercise Rehabilitation.” BMC Sports Science, Medicine and Rehabilitation, vol. 14, no. 1, 7 Feb. 2022, p. 18, www.ncbi.nlm.nih.gov/pmc/articles/PMC8819209/, https://doi.org/10.1186/s13102-022-00407-3.